Data insight:
COVID-19 trends in the United States
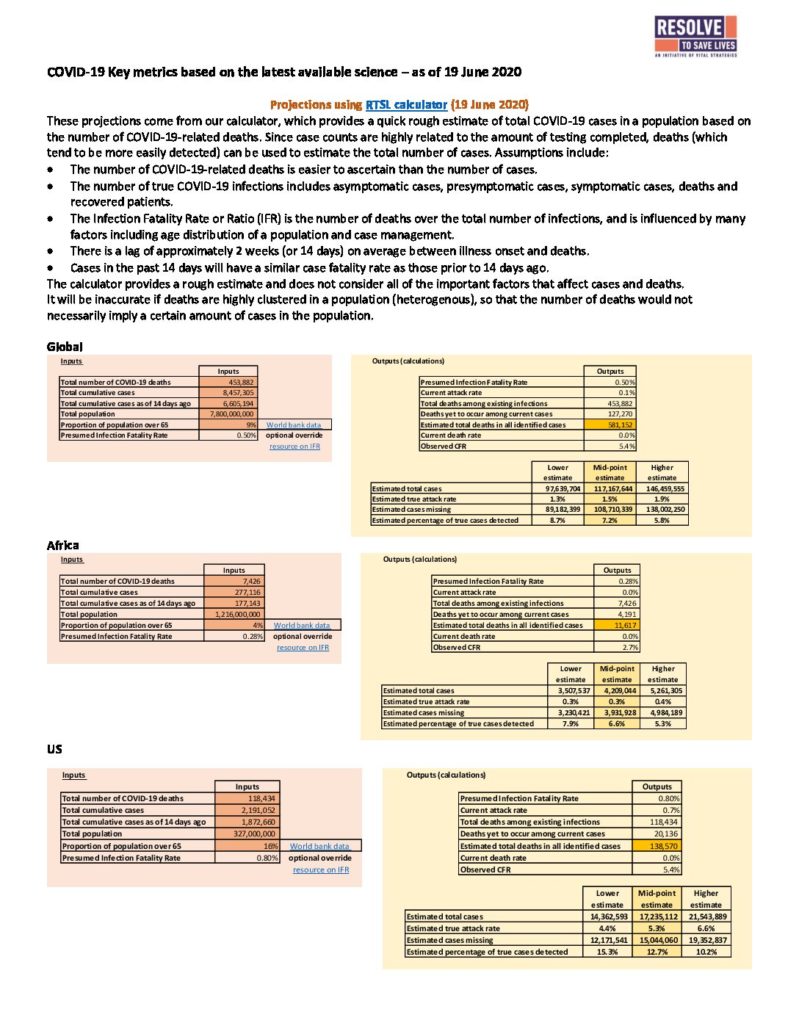
In a previous Data Insight, we highlighted key indicators to monitor as US states were beginning to reopen their economies and scale back public health and social measures (PHSM). Continuous monitoring and frequent periodic assessments of key indicators allow for data-driven, evidence-based policymaking in the effort to protect residents and resume social and economic activity during the ongoing pandemic. The need to loosen and tighten restrictions may be a reality around the world for months to come. The response to the COVID-19 pandemic is most effective when public health and economic factors are considered in concert with one another, saving both lives and livelihoods.
The pandemic has affected all of the United States, but its impact has been different in both character and magnitude from one city, state or county to the next. The prior Data Insight on resurgence focused on what we can learn by monitoring trends in mobility, surveillance of typical COVID-19 signs and symptoms (syndromic surveillance), case counts, hospitalizations and deaths in the larger context of increased testing capacity and adjusting PHSMs. We normally expect to see an increase in mobility and cases ahead of increases in hospitalizations and deaths, given the lag time that is an inherent in the progression from exposure and infection to illness and death. This lag between exposure and the reported death can be as long as four weeks. In this Data Insight, we examine five US states different geographic and epidemiological characteristics and look specifically at what their COVID-19 indicators show since the states took steps to reopen their economies.
| State | Began relaxing PHSMs | Mobility | Syndromic | New Cases | Testing | Test Positivity | Hospitalizations | Death |
|---|---|---|---|---|---|---|---|---|
| Arizona | May 15 |  |  |  |  |  |  |  |
| California | May 8 |  | N/A |  |  |  |  |  |
| Maryland | May 15 |  | N/A |  |  |  |  |  |
| Oregon | May 15 |  |  |  |  |  |  |  |
| Texas | May 1 |  | N/A |  |  |  |  |  |
Read the full Data Insight with details on the five states examined.
In-depth topics
Face mask update
Since SARS-CoV-2 was identified, information about how the virus is transmitted and how to protect against it has been accumulating. Even so, many key questions have yet to be fully answered. As the pandemic spreads rapidly with devastating impact, public health officials have been compelled to advance recommendations in the face of this incomplete and shifting knowledge. At times this has resulted in changing, even conflicting, policies and risk communication. Guidance on the use of face masks in the general population has varied over time and from place to place—perhaps more so than for other public health and social measures. Global and national guidance on face mask use in the general population have occasionally been at odds. In some cases, policies have shifted within weeks, or seemed to reverse prior positions.
Early in the pandemic, many subject matter experts expected that SARS-CoV-2 transmission would be similar to other common respiratory viruses. When community transmission was first described, data suggested that people in close contact with symptomatic case patients could contract the infection by inhaling infected particles or touching contaminated surfaces. Most public health authorities recommended widespread physical distancing, limitations on mass gatherings, cough hygiene, hand washing and avoiding touching one’s face. Few advised the general public to use face coverings, except in settings where cultural practices already favored mask use. Masks were recommended as personal protective equipment for health workers and first responders, for people with symptoms, and for people caring for patients with COVID-19 at home. Ensuring enough masks would be available for these groups was also a priority and may have tempered enthusiasm for recommending more widespread use, especially while supplies were scarce. That was not the only concern. Until earlier this month, the World Health Organization cautioned that universal mask use had not been proven to protect healthy people from becoming infected with COVID-19 and could lead people to touch their faces more frequently or discontinue other measures such as physical distancing.
Over time, incremental evidence showed how easily COVID-19 could be transmitted. Epidemiological and laboratory studies demonstrated that viral load is highest early in illness and before symptom onset, that viral particles could remain infectious after being suspended in the air, and indicated that people who were infected with the virus contributed to transmission, even when they didn’t have symptoms. Some observers suggested that widespread community use of face masks may have contributed to the ability of some countries and areas, including the Republic of Korea, Taiwan and Hong Kong, to mitigate the impact of their COVID-19 epidemics. By early April, US officials began recommending face masks for the general public, and some jurisdictions mandated them. In a recently published review COVID-19 case rates grew more slowly in 15 states and the District of Columbia that had mandated universal public face mask use before April 1, 2020. The authors estimate that these measures may have prevented 230,000 to 450,000 cases of COVID-19 by May 22.
Recommendations can address three types of face masks. Respirators (including N95 and KN95) and medical procedure masks, also called surgical masks, are manufactured from nonwoven materials to precise specifications and are specifically recommended for health workers. There is evidence from laboratory simulations and controlled trial studies to show that these types of masks can contribute to reducing infection of respiratory viruses and other pathogens in health care settings if they are used by health care workers properly and consistently. Cloth face coverings, which can include commercial, home sewn or improvised barriers, have also been recommended for the general population. These are more affordable and accessible than respirators and medical procedure masks, which should be prioritized for specific high-risk settings such as health care. Cloth face coverings don’t meet the same standards required for respirators and medical procedure masks, and are not as effective as surgical masks in studies with health workers. In addition, cloth masks have been associated with higher risk of infection due to moisture retention, reuse of cloth masks and poor filtration may result in increased risk of infection. There is evidence that when sick patients wore face masks, including cloth face coverings, they were less likely to infect healthy people with whom they had contact. If worn by a large proportion of the general population and combined with other public health and social measures, face masks can reduce the incidence of other respiratory infections in a community, particularly when deployed early in an outbreak or transmission season. We previously covered in our Weekly Science Review a meta-analysis of data from 172 observational studies that concluded face masks could have a large impact specifically on reducing COVID-19 and related viruses causing SARS and MERS (aOR=0.15). In a recent mathematical model, investigators demonstrate that even imperfectly effective masks (that block only 20% of transmission) could be of high value in curtailing the burden of COVID-19, when consistently used by a high enough proportion of people and combined with other measures including physical distancing.
Most of the systematic reviews that examined effectiveness of face masks include a mix of studies, including many that fail to show an impact, and rely heavily on low-certainty data from observational studies and non-randomized designs that included multiple interventions at once. Even so, evidence, expert opinion and guidance are converging. WHO now recommends widespread community mask use as part of a package of public health and social measures and CDC recently advised people to use face coverings in its revised guidance for mass gatherings and events. But some people remain confused and others may have lost confidence in recommendations that seem to have shifted over time. In the United States, where public support for strict containment measures has become increasingly polarized, the face mask has become a partisan symbol of support for or defiance of public health authorities. Similar resistance has characterized previous public health crises. During the 1918 Spanish influenza, anti-mask leagues were formed in some US cities, notably San Francisco. As many communities, states and countries open and relax some restrictions imposed to curb the spread of COVID-19 and more and more people resume activities outside the home, the use of face masks in public may be more important than ever. One recent mathematical modeling study concludes that widespread face mask use and physical distancing will be key to reopening economic activity and limiting the need for future lock-downs. Given that perspective, there’s good reason to reclaim face coverings as a symbol of liberation, and encourage everyone to observe the 3 W’s for a safer reopening: Wear a mask, Wash your hands (or use hand sanitizer), and Watch your distance.
Fecal transmission of COVID-19
The virus that causes COVID-19, SARS-CoV-2, is considered a respiratory virus because it typically infects the respiratory tract, including the airways and/or lungs, and causes respiratory symptoms. SARS-CoV-2 can also infect cells in other parts of the body, just as other respiratory viruses do. SARS-CoV-2 enters host cells via a cell receptor called angiotensin converting enzyme II (ACE2). This receptor is found on cells in the respiratory tract as well as on cells in the gastrointestinal tract. Gastrointestinal symptoms among COVID-19 patients have been widely reported. In a review on the incidence of gastrointestinal symptoms among patients with COVID-19, of more than 4,000 patients included in the analysis, 7.4% reported diarrhea and 4.6% reported nausea or vomiting. In a review that pooled results of stool testing for SARS-CoV-2 genetic material (ribonucleic acid, or RNA), 291 (53.9%) of 540 COVID-19 patients tested positive. The reasons for conducting stool testing were not always specified; it is possible that a relatively high proportion of tested patients had gastrointestinal symptoms and the results may not be typical of all infections. In the same review, 125 (62.8%) of 199 patients who underwent serial stool testing showed persistent shedding of viral particles in stool after a negative respiratory sample, and the duration of stool viral shedding after respiratory samples turned negative ranged from 1 to 33 days.
Thus, it is reasonable to ask whether stool poses an infectious risk. There are several theoretically possible transmission routes. One is the fecal-oral route, in which stool is ingested (by, for example, consumption of contaminated food) and cells in the gastrointestinal tract serve as the viral entry point. Another possibility is transmission via fomites, if someone touches a surface contaminated with stool particles and then touches their nose or eyes. A third is airborne transmission, as flushing a toilet may generate aerosols. During the 2003 severe acute respiratory syndrome (SARS) outbreak in Hong Kong, aerosolization of toilet water may have contributed to disease spread. In order for the SARS-CoV-2 in stool to pose an infection risk in any of these circumstances, live virus—not just genetic material—must be present. It has been suggested by experiments examining the effect of simulated human colonic fluid on viral viability that the SARS-CoV-2 shed in feces is unlikely to be capable of causing infection. However, studies have demonstrated that live virus can be detected in the stool of COVID-19 patients, albeit in a minority of samples assessed. In one study, live SARS-CoV-2 was isolated from 1 of 4 fecal samples from a COVID-19 patient. In another study in which 44 patients had evidence of SARS-CoV-2 RNA in their stool, electron microscopy suggested the presence of live virus in two stool samples. In Guangzhou, China, it was reported that water contaminated by the feces of a COVID-19 patient that leaked from a ruptured sewage pipe was the likely source of infection for six new cases.
Fecal shedding of SARS-CoV-2 may be useful to public health efforts to track disease spread, via monitoring of sewage for SARS-CoV-2. It has been reported that over 250 wastewater treatment facilities in 40 states and a number of other countries are conducting wastewater testing for SARS-COV-2. Wastewater-based epidemiology (WBE), as this type of research may be called, has been successfully used to provide early warning of outbreaks of other diseases. In several European cities, SARS-CoV-2 RNA has been detected in city wastewater collected before any local cases were reported. The amount of SARS-CoV-2 genetic material may also indicate the true spread of the epidemic and enable determination of whether disease incidence is increasing or decreasing. A study in Paris, France, showed that the increase of SARS-CoV-2 genetic material in raw wastewater was correlated with the increase of human COVID-19 cases.
Dexamethasone use in those with severe COVID-19 illness
The University of Oxford issued a press release on June 16 about preliminary findings of a randomized clinical trial on potential treatments for COVID-19. The data has yet to be released, and neither a preprint nor peer-reviewed report is available. For the first time since the start of the COVID-19 pandemic, a team of researchers has reportedly identified a medication that may improve survival in some COVID-19 patients. The medication is dexamethasone, a synthetic steroid. Steroid medications have been extensively studied as potential treatments for patients with serious respiratory illnesses. Dexamethasone is cheap and widely available and has long been in the armamentarium of doctors across the world. Although the study, called the RECOVERY (Randomised Evaluation of COVid-19 thERapY) trial, is examining a number of other treatments and is yet to be completed, the dexamethasone component of the study was halted on June 8 when it was determined by an oversight committee that enough data had been collected to determine whether or not dexamethasone had benefit.
Synthetically produced steroids imitate hormones that are naturally produced in the body in the adrenal glands. Steroids help regulate many processes in the body, and in certain doses, can act as anti-inflammatory compounds by quelling the body’s immune system. There are several types of steroids that are used for various conditions, ranging from asthma to lupus to rashes, but some steroids have been of special interest to doctors who manage critically ill patients with sepsis and acute respiratory distress syndrome (ARDS), a severe respiratory condition that can occur in COVID-19 patients. It is thought that by countering an exaggerated immune response which can be triggered by some infections and result in a storm of damage to the tissues in the lung, steroids can improve outcomes for patients with severe respiratory illness. Steroids treatment is not without risks because the body needs its immune response to fight off infections. Balancing the benefit steroids may offer against the risk of worsened infections and other complications can be delicate. Although steroids may benefit some patients with ARDS and patients with certain types of respiratory infections, there is concern that steroids may harm COVID-19 patients. This stems in part from the long and complex history of research on steroids for respiratory infections; some studies have shown benefit while others have shown harm. Of particular note are studies on patients with other coronavirus diseases, severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS), which have generally shown that steroids are either of no benefit or may cause harm.
According to the press release on the RECOVERY trial, over 11,500 COVID-19 patients have been enrolled from over 175 hospitals in the United Kingdom. A total of 2,104 patients received dexamethasone for ten days and were compared with 4,321 patients who received usual care. After one month, mortality rates among the patients who received usual care were as follows: 41% of patients who required ventilation had died, 25% of those who required oxygen had died, and 13% of those who did not require respiratory support had died. Dexamethasone reduced deaths by one-third in ventilated patients and by one-fifth in patients receiving oxygen only; there was no benefit among patients who did not require respiratory support. These data would suggest that dexamethasone can save one life for every eight of the sickest patients treated. In other studies when steroids have been shown to confer benefit, this has typically been observed in specific subsets of patients. In addition, timing of steroid administration in the course of disease can be important. The full release of trial results is eagerly awaited.
Weekly Research Highlights
Coronavirus Disease 2019 Case Surveillance – United States, January 22 – May 30, 2020
(MMWR Early Release 15 June)
- All 50 US states, New York City, and the District of Columbia submitted data on residents testing positive by RT-PCR for SARS-CoV-2, the virus that causes COVID-19. As of May 30, 1,761,503 cases and 103,700 deaths were reported. Researchers continue to examine this data for trends in demographics, severe outcomes and clinical information.
- Cumulative incidence per 100,000 population was highest among those over 80 years of age (902), followed by those 50-59 years of age (550.5) and those 40-49 years of age (541.6). Cumulative incidence per 100,000 was lowest for those under 10 years of age (51.1). Among a subset of patients for whom hospitalization data was available, 14% were admitted to the hospital, with 2% in the ICU.
- Surveillance data is limited in its ability to fully capture all data points completely, and data on symptoms, race, or other demographics may not be captured adequately or be representative.
The impact of COVID-19 and strategies for mitigation and suppression in low- and middle-income countries
(Science June 12, 2020)
- Researchers examined available data on population size, age distribution, social contact patterns, comorbidities, and health care quality and availability for 121 countries. They developed an age-structured modelling framework to examine how health system capacity constraints in different settings would affect the epidemic and the most effective responses under 2 scenarios:
- Mitigation—where transmission is reduced but not eliminated (Rt>1.0), resulting in an epidemic that declines following a single peak as herd immunity develops.
- Suppression—where transmission is minimized and brought to very low levels (Rt<1.0) such that herd immunity does not develop and transmission will rise if interventions are later released.
- Even with optimal social distancing and a young population, under the mitigation scenario, peak demand for critical care in a typical low-income country would outstrip supply by a factor of 30.7 (95% UI, 14.7 – 48.8).
- In suppression scenarios, if interventions are not maintained, low- and lower middle-income countries could experience a lower burden per-capita, due primarily to the younger population. The models predict that the poorer quality of health care available in these countries is likely to have a greater impact on the overall infection fatality rate than the absolute limits on capacity alone.
- Complex decisions about how to respond will have to be made locally. Priority should be given to increasing oxygen support to mitigate the health impact of COVID-19, along with enhancing testing and surveillance to reduce spread and tailor other mitigation and suppression interventions.
- The authors note important limitations of their approach including the lack of reliable data from LMICs and having to make assumptions based on observations or consensus estimates developed elsewhere.
Suggested citation: Cash-Goldwasser S, Kardooni S, Cobb L, Bochner A, Bradford E and Shahpar C. In-Depth COVID-19 Science Review June 13 – 19, 2020. Resolve to Save Lives. 2020 June 23. Available from https://preventepidemics.org/covid19/science/review/