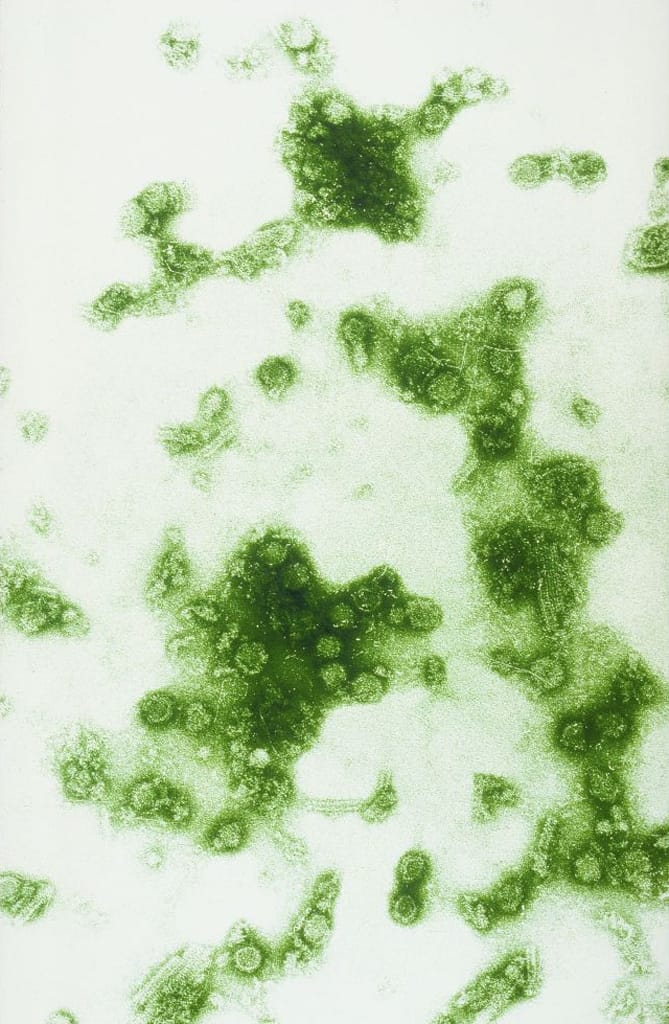
About Dengue
Endemic in more than 100 countries, dengue is a viral disease transmitted to humans through mosquito bites.1 Globally, dengue is on the rise—there were more than 5 million reported cases in 2019, compared to about 500,000 in 2000; some experts estimate the true number of dengue infections to be nearly 400 million each year.2,3 Although it primarily affects people living in the tropics, due to climate change, the primary mosquito that carries it—Aedes aegypti4—has spread northward, and cases have been reported in Europe and the United States in recent years.5 Worldwide, dengue causes about 20,000 deaths per year—most of which are children.6
Many dengue cases are mild and can be asymptomatic. Those who do become ill experience symptoms such as headache, nausea, fever and severe joint pain, hence its common name: breakbone fever. About 5% of those infected experience severe dengue, which can include bloody or continuous vomiting and severe abdominal pain.7 Severe dengue can cause substantial bleeding or organ impairment, and it can be fatal when not managed with proper medical care. Use of early treatment methods such as intravenous therapy can keep the mortality rate lower than 1%.8
Globally, dengue is on the rise—there were more than 5 million reported cases in 2019, compared to about 500,000 reported cases in 2000.
Dengue prevention measures include mosquito surveillance, clearing mosquito breeding sites—which tend to be near stagnant water—and wearing more clothing to minimize risk of exposure to mosquitos. Because Aedes aegypti mosquitos are most active during the day, mosquito bite prevention tools such as bed nets are not necessarily effective with dengue.

What Happened
On December 5, 2021, a resident of Sobokerto, Indonesia—an agricultural village outside of Surakarta—arrived at a local hospital with distressing symptoms. The resident had been suffering with fever and joint pain; red spots were also detected on the skin. The area where the resident lived, with many ponds and in the middle of its rainy season, was on high alert for dengue. Hospital staff tested for dengue, and within a few days, the test result came back positive.

The Response
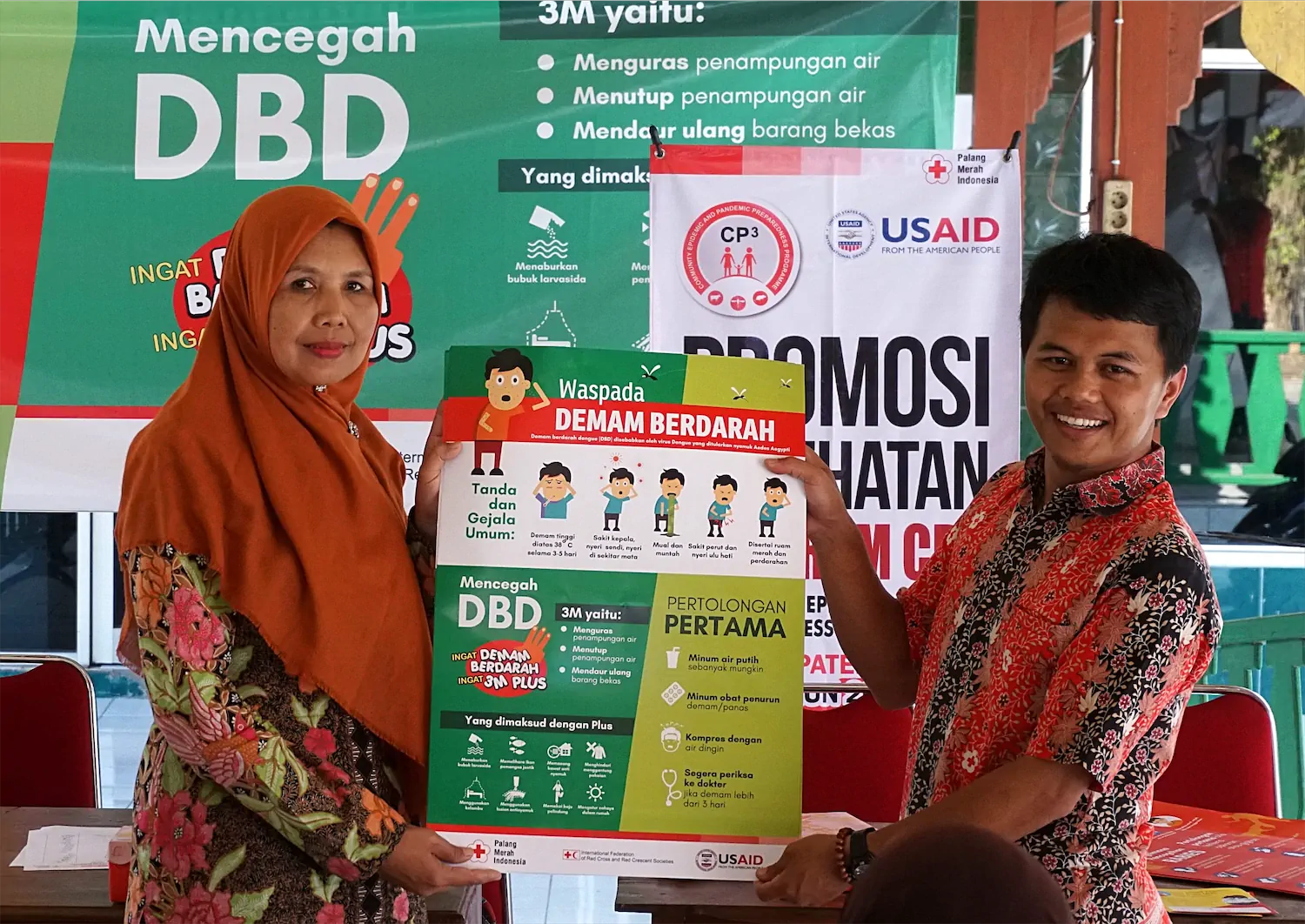
The resident’s family had taken them to the hospital on the advice of Red Cross volunteers in the village. These volunteers were members of the local community who had been trained in community-based surveillance (CBS) through the Community Epidemic & Pandemic Preparedness Programme (CP3).9 They visited the resident at home and confirmed that the community case definition of dengue had been met. A community case definition of a disease is a simplified, observational form of disease examination that trained volunteers with no medical background can perform with reference to a small set of easily identifiable symptoms.10 The volunteers reported the case to the village midwife immediately and used a mobile-based data collection tool to report the case to their district supervisor.


At the same time, the volunteers launched risk communication and community engagement activities to reduce the risk of further infections. Initially, this meant going door-to-door to notify families that there was a potential dengue case in the village and providing education on dengue prevention. Most local families knew how to clean their bathrooms to prevent a mosquito infestation; however, the volunteers found that families did not know as much about other threats of mosquito breeding. Open sewage systems, unclean water storage units, open-air waste disposal areas and even bamboo groves—popular play areas for children—can accumulate stagnant puddles of water and thus attract mosquitos. The volunteers mapped out the community’s environmental risk by identifying potential breeding sites and then worked with the community to eradicate them. Red Cross volunteers were well-placed to communicate with local families about disease risks and how to manage them because, unlike an outside health authority that might visit during an outbreak, they were known and trusted by the people in the communities in which they lived and served.
To spread the word more widely in the community, the volunteers spoke at local events such as religious services, youth groups and the Posyandu—a monthly maternal and child care service organized by the local health authority. As a large gathering of mothers, who, the volunteers noted, are “the spearheads of household health,” the Posyandu was a particularly helpful venue for discussing dengue prevention measures.
The resident who was diagnosed with severe dengue returned home from the hospital on December 10 and fully recovered. No further dengue cases were reported in the area.
The Red Cross volunteers’ quick actions followed best practices for dengue mitigation. They were practicing CBS, in which non-medically trained community members are taught to recognize signs of high-risk infectious diseases, report them to the appropriate authorities and deliver the disease-related information to the community as early response. CBS champions the value of communication about disease risks from trusted sources—one’s fellow neighbors—and trains participants to conduct peer-to-peer education. CBS enables volunteers to connect communities to health services, identify potential outbreaks and take preventive actions.

The Red Cross trained volunteers on identifying health risks based on signs and symptoms. For example, a suspected community case of dengue can be identified if a patient experiences fever and joint pain, as well as two or more other symptoms (including red spots). Although not a medical diagnosis—which can only be carried out by a trained health professional—evidence-based community case definitions can allow non-medically trained volunteers to identify signs and symptoms early and refer patients to seek care and evaluation by health professionals; they also provide the means to trigger early preventive actions more rapidly than through a traditional surveillance system. A survey of 31 community-based surveillance alerts for dengue in Indonesia between Sept 2019 and Sept 2020 found that all but three were later confirmed via laboratory diagnosis.11
Key Preparedness Factors
- Risk Assessment & Planning
- Emergency Response Operations
- National Laboratory System
- Disease Surveillance
- National Legislation Policy & Financing
- Human Resources
- Risk Communications
Bottleneck
An outbreak response is multifaceted and coordinated across a range of sectors and actors. Relative weaknesses can lead to bottlenecks that delay or otherwise impair response efforts. These bottlenecks can be identified via after-action reviews and are valuable intel for improving future response efforts.
Facilitator
A disaster never happens because a single thing goes wrong. Bottlenecks or other system weaknesses are often balanced by facilitators—factors that strengthen response efforts. Facilitators can also be identified via after-action reviews and may be the direct result of system improvements following the identification of bottlenecks.
References
- World Health Organization. (2022, January 10). Dengue and Severe Dengue. https://www.who.int/news-room/fact-sheets/detail/dengue-and-severe-dengue
- World Health Organization. (2022, January 10). Dengue and Severe Dengue. https://www.who.int/news-room/fact-sheets/detail/dengue-and-severe-dengue
- Centers for Disease Control and Prevention. (2021, September 23). About Dengue: What You Need to Know. https://www.cdc.gov/dengue/about/index.html
- World Health Organization, Regional Office for Europe. (2013, February 4). Infectious Diseases in a Changing Climate. https://www.euro.who.int/__data/assets/pdf_file/0009/234198/Dengue-in-the-WHO-European-Region.pdf
- European Centre for Disease Prevention and Control. (2021, March 4). Factsheet about Dengue. https://www.ecdc.europa.eu/en/dengue-fever/facts
- Mayo Clinic. Dengue Fever. https://www.mayoclinic.org/diseases-conditions/dengue-fever/symptoms-causes/syc-20353078
- Jog S, Kulkarni A, Kalyani P. (2018). How to Manage Severe Dengue Infection. ICU Management & Practice, Volume 18 – Issue 4, 2018. https://healthmanagement.org/c/icu/issuearticle/how-to-manage-severe-dengue-infection
- Centers for Disease Control and Prevention. (2021, December 20). Vaccine Eligibility & Recommendations. https://www.cdc.gov/dengue/vaccine/hcp/eligibility/index.html
- In Indonesia, the Community Epidemic and Pandemic Preparedness Program (CP3) is led by the Indonesia Red Cross Society, with support from the International Federation of Red Cross and Red Crescent Societies and the United States Agency for International Development (USAID). CP3 recognizes that early information about outbreaks often reaches standard surveillance systems late and works to connect communities with national health and surveillance.
- Republic of Uganda Ministry of Health. (September 2021). National Technical Guidelines for Integrated Disease Surveillance and Response, Third Edition. https://www.afro.who.int/sites/default/files/2021-09/2_Uganda%203rd%20IDSR%20Tech%20Guideline_PrintVersion_10Sep2021.pdf
- International Federation of Red Cross and Red Crescent Societies, Palang Merah Indonesia. (April 2021). Community-Based Surveillance, Indonesian Red Cross experience. https://www.ifrc.org/sites/default/files/CaseStudy_Indonesia_CommunityBasedSurveillance_IFRC-PMI04-2021_short.pdf