About Monkeypox
Monkeypox is a rare viral disease closely related to cowpox and smallpox. Although the virus was identified in 1958 in a group of monkeys used for research, rodents and primates appear to be the main animal carriers of the virus.1 The first human case was identified in 1970 in the Democratic Republic of Congo (DRC); most human cases have emerged in West and Central Africa, although outbreaks have also occurred in the United States, United Kingdom and Israel in recent years.2
While there is some human-to-human spread, the primary mode of transmission is through contact with infected animals. Symptoms include fever, rash, swollen lymph nodes and painful blisters, similar to those caused by smallpox. In severe cases, monkeypox can be fatal; it has a fatality rate of up to 11%.3 The smallpox vaccine is 85% effective against monkeypox, but the vaccine has not been widely used since 1980, when smallpox was eradicated.4 There is no other vaccine or medicine to prevent or treat monkeypox.
Although monkeypox remains rare, it has become more common since the 1980s. From 1981 to 1986, 404 cases were identified across Africa. In the DRC,5 where most of the world’s cases occur, there have been more than 1,000 cases per year since 2005,6 and 4,594 cases were reported from January to September 2020 alone.

What Happened
After 39 years with no reported cases of monkeypox, Nigeria’s largest outbreak took place in 2017.7 Between 2017 and 2019, more than 300 cases were reported.8 Until September 2019, most of those cases had been limited to Lagos and Delta states on the Nigerian coast.
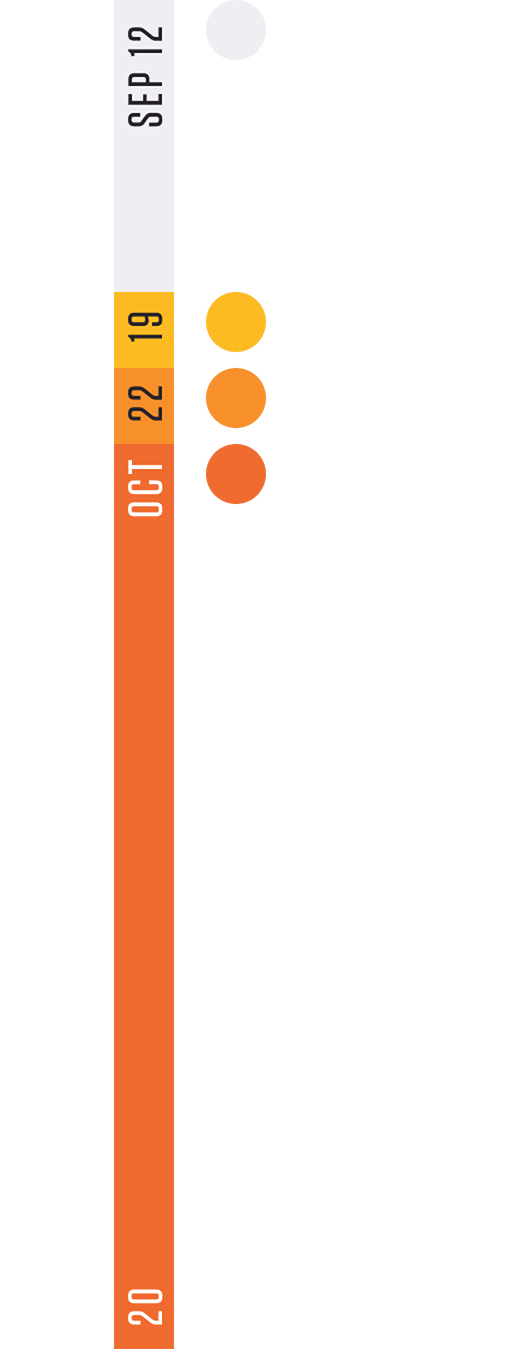
On September 12, 2019, a suspected case of monkeypox was identified for the first time in Akwa Ibom, a state on Nigeria’s eastern coast. Ten days later, the diagnosis was confirmed by laboratory testing. Although there had been monkeypox cases in surrounding states, the confirmed case, along with nine other suspected cases, were the first cases in Akwa Ibom, and authorities were alarmed about the possibility of further spread.
Officials also moved to categorize monkeypox as an infection requiring immediate reporting to national authorities for faster alerts and response.

The Response
Years of preparation by Nigeria health officials ensured that they were ready to fight the new outbreak in Akwa Ibom state. When monkeypox first reappeared in Nigeria in September 2017, the Nigerian Centre for Disease Control (NCDC) published national guidelines for outbreak response.9 Officials also moved to categorize monkeypox as an infection requiring immediate reporting to national authorities for faster alerts and response. NCDC provided rapid response teams anywhere there were confirmed cases and undertook extensive communications to educate the public about the virus and its risks.10
The national rapid response team sent to assist local and state authorities joined state public health and laboratory officials to address the outbreak together. The combined team worked to identify additional cases, carried out contact tracing and supported improved surveillance, case management and sample collection methods. Poor sample collection from the initial suspected cases meant that, aside from the single positive, other test results were inconclusive. In total, the rapid response team identified eight more suspected cases, all of whom tested negative. Of the 18 total suspected cases, only one was laboratory confirmed.
Key Preparedness Factors
The rapid response team also conducted surveys to understand awareness of monkeypox among clinicians in Akwa Ibom. Results showed a strong understanding of the virus and how to identify and manage it, but weakness in sample collection protocols and high levels of stigma toward patients. In response, local medical personnel were provided with training in sample collection and education to reduce stigma. Other gaps were identified at the local infectious disease hospital, and recommendations were made for further improvements. Teams also ran education campaigns to counter the stigma against infected people that was prevalent throughout the community.
The rapid response team supported the state to take full ownership of the outbreak response, improve surveillance and continue efforts to reduce stigma toward those infected with monkeypox. Further, the team urged Akwa Ibom state to more proactively ensure that cases were taken to the local infectious disease hospital, which was hindered by a lack of funds to fix a broken ambulance and the run-down state of the hospital.11

Thanks to the swift action taken by the Ministry of Health and local authorities, the outbreak in Akwa Ibom had been contained within a month’s time.

At the end of the rapid response team’s visit, the Akwa Ibom state’s commissioner for health communicated to the community about the outbreak, asking them to avoid contact with animals that could harbor the virus and to avoid touching anything that had been in contact with infected animals. People were also asked to self-quarantine while health officials collected samples and sent them for testing.12
The rapid response teams and the collaboration between state and national experts led to the quick and thorough outbreak response. Thanks to the swift action taken by the Ministry of Health and local authorities, the outbreak in Akwa Ibom had been contained within a month’s time.
This case study was developed in partnership with the Akwa Ibom State Ministry of Health and the Nigeria Centre for Disease Control.
Timeline

The ability of the state to respond quickly to this outbreak showcases what is possible when we make the right investments in public health.
Dr. Nsisong Asanga, Field Epidemiologist
References
- World Health Organization. (2019, December 9). Monkeypox. https://www.who.int/news-room/fact-sheets/detail/monkeypox
- Federal Ministry of Health - Nigeria Centre for Disease Control. (2017). Interim National Guidelines for Monkeypox Outbreak Response. https://ncdc.gov.ng/themes/common/docs/protocols/50_1508912430.pdf
- World Health Organization. (2019a, November 1). Monkeypox. https://www.who.int/health-topics/monkeypox/
- World Health Organization. (2019a, November 1). Monkeypox. https://www.who.int/health-topics/monkeypox/
- World Health Organization. (2020, October 28). Monkeypox – Democratic Republic of the Congo. https://www.who.int/csr/don/01-october-2020-monkeypox-drc/en/
- Centers for Disease Control and Prevention. (2019). About Monkeypox | Monkeypox | Poxvirus | CDC. https://www.cdc.gov/poxvirus/monkeypox/about.html
- Chieloka, O. S., Amao, L. K., Akinrogbe, J. T., Iniobong, J.-I. & Burga, J. (2020). Outbreak Investigation of Monkeypox in Akwa Ibom State: A Matched Case Control Study 14th -24th October 2019. East African Journal of Health and Science. 1(1), 37-44. https://journals.eanso.org/index.php/eajhs/article/view/57
- Chakrabarti, S., Clarke, S., & Boggild, A. (2019, June 4). Monkeypox outbreak in Nigeria. On Medicine. https://blogs.biomedcentral.com/on-medicine/2019/06/04/monkeypox-outbreak-in-nigeria/#:~:text=The%20outbreak%20continues%20in%202019,had%20received%20preventative%20smallpox%20vaccination
- Federal Ministry of Health - Nigeria Centre for Disease Control. (2017). Interim National Guidelines for Monkeypox Outbreak Response. https://ncdc.gov.ng/themes/common/docs/protocols/50_1508912430.pdf
- Federal Ministry of Health - Nigeria Centre for Disease Control. (2017). Interim National Guidelines for Monkeypox Outbreak Response. https://ncdc.gov.ng/themes/common/docs/protocols/50_1508912430.pdf
- Chieloka, O. S., Amao, L. K., Akinrogbe, J. T., Iniobong, J.-I. & Burga, J. (2020). Outbreak Investigation of Monkeypox in Akwa Ibom State: A Matched Case Control Study 14th -24th October 2019. East African Journal of Health and Science. 1(1), 37-44. https://journals.eanso.org/index.php/eajhs/article/view/57
- Anthony, L. (2019, October 26). 18 cases of monkey pox reported in Akwa Ibom. Daily Post Nigeria. https://dailypost.ng/2019/10/26/18-cases-of-monkey-pox-reported-in-akwa-ibom/
