About Ebola
Ebola Virus Disease is a rare but deadly disease caused by a virus transmitted initially from animals to humans. Bats are thought to be the natural host to the disease, and initial infection can occur when humans come in contact with a bat or eat an animal that has been infected by a bat.1 An outbreak of Ebola can occur when an infected person spreads the virus via bodily fluids to other humans. Since Ebola’s discovery in 1976, death rates have ranged from 25% to 90% during outbreaks. While there have been relatively few outbreaks, the most devastating occurred in 2014-2016 in several countries in West Africa, infecting around 28,600 people and killing approximately 11,325.2

Initial symptoms can be similar to the flu, but later stages include poor liver and kidney function and internal and external bleeding.3 Supportive treatment, such as oral or intravenous fluids, dramatically improves chances of survival, and a treatment was approved in 2020.4 Effective vaccines have been available since 2019, but supply remains limited, and there are significant logistical challenges for delivery.5

What Happened
B eginning in August 2018, an Ebola outbreak took hold in North Kivu and Ituri, provinces of DRC. Ongoing conflict in the area severely hampered the response, and the virus was able to spread widely. By the time the outbreak in DRC was over in June 2020, 3,481 people had been infected, and 2,299 died, making it the second largest outbreak of Ebola to date. Its 66% case fatality was relatively high compared to other outbreaks. 6, 7 DRC’s North Kivu and Ituri provinces border Western Uganda. Given the sizable outbreak in DRC and the movement of large numbers of citizens and refugees across the border, Uganda was at high risk for international spread.
Having prepared for an Ebola outbreak since August 2018, Uganda rapidly mobilized its response teams.
In early June 2019, a five-year-old boy tested positive for Ebola at the Bwera Hospital in Kasese district, Uganda, close to the DRC border. The child had recently traveled with family to DRC for the burial of his grandfather, who had died from Ebola. Within days, the boy and two other members of the family, a grandmother and three-year-old brother who also tested positive for Ebola, had died.8 The Ministry of Health declared the outbreak on June 9, 2019, and instituted response measures to stop any spread.
However, the boy and his family were the first of only a handful of cases that were reported in Uganda during the entire outbreak in DRC, despite millions of border crossings between the two countries. No further cases spread in Uganda from these individuals.
Key Preparedness Factors
The Response
Having prepared for an Ebola outbreak since August 2018, Uganda rapidly mobilized its response teams.
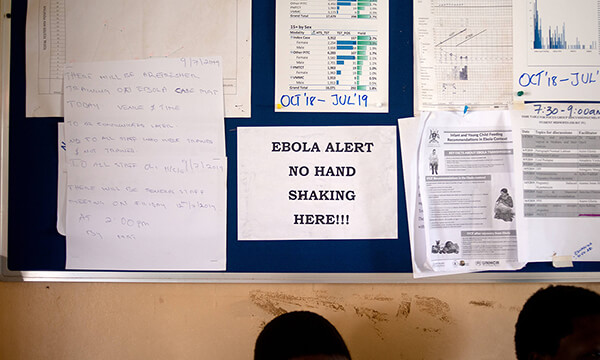
Within days of the Ebola outbreak being declared in DRC in August 2018, Uganda activated its national emergency preparedness and response systems. Within weeks, Uganda opened multiple Ebola Treatment Centres and rapid testing laboratories near the DRC border, where border screenings were conducted for all people entering the country.9 By November 2018, the Ugandan government had vaccinated nearly 5,000 health care workers and response staff—all before any cases had been identified in Uganda.10
When the five-year-old boy and his family returned to Uganda from DRC in June 2019, they were quickly identified at a routine Ebola screening point at Mpondwe border crossing, tested, and then placed in an Ebola Treatment Centre once confirmed positive.11 Because the Ugandan government had set up field laboratories capable of testing for Ebola in the area, test results were available within six hours and confirmed via additional testing within 24 hours.
The national and district emergency response team was immediately convened to reinforce response activities, including scaling up risk communications and vaccinating nearly 300 contacts of the cases.12 No further infections were identified, and the outbreak was declared over on July 25, after the recommended 42-day period with no new cases had elapsed.13
Uganda’s extensive border screenings identified several individuals with suspected Ebola symptoms; they were isolated and tested, with test results often returned within 24 hours. Apart from the boy and his family, only two other positive cases emerged during the DRC epidemic, both of which were quickly identified, investigated and managed, avoiding further infections.14, 15
The quick activation of Uganda’s health emergency response systems—in place long before Ebola cases in DRC threatened an outbreak in Uganda—prevented any further infections.
This case study was developed in partnership with the Infectious Diseases Institute, Makerere University.

We thank all the stakeholders including donors, implementation partners and local communities for working quickly with the response mechanism to ensure that the cases were detected early, contacts managed well and no secondary cases emerge. As a country we are proud to have this outbreak closed.
Hon. Minister of Health of Uganda, Dr. Jane Ruth Aceng
Timeline

The speed and enthusiasm of the teams, the leadership and commitment from national to district and community level are commendable in this Ebola outbreak response. We need to continue being vigilant and detect any cases early to avoid large outbreaks in Uganda. WHO will continue supporting the country to build resilience capabilities and systems that ensure health security for all.
WHO Country Representative to Uganda, Dr. Yonas Tegegn Woldemariam
References
- World Health Organization. (2021b, February 23). Ebola virus disease. WHO. https://www.who.int/news-room/fact-sheets/detail/ebola-virus-disease
- Centers for Disease Control and Prevention. (2019). 2014-2016 Ebola Outbreak in West Africa | History | Ebola (Ebola Virus Disease) | CDC https://www.cdc.gov/vhf/ebola/history/2014-2016-outbreak/index.html
- World Health Organization. (n.d.). Frequently asked questions. WHO. https://www.who.int/emergencies-old/diseases/ebola/frequently-asked-questions
- U.S. Food and Drug Administration. (2020, October 14). FDA Approves First Treatment for Ebola Virus. https://www.fda.gov/news-events/press-announcements/fda-approves-first-treatment-ebola-virus
- World Health Organization. (2020, February 14). Four countries in the African region license vaccine in milestone for Ebola prevention. https://www.who.int/news/item/14-02-2020-four-countries-in-the-african-region-license-vaccine-in-milestone-for-ebola-prevention
- World Health Organization. (2021a, January 12). Ebola outbreak 2018-2020- North Kivu/Ituri, DRC. https://www.who.int/emergencies/diseases/ebola/drc-2019
- World Health Organization. (2021b, February 23). Ebola virus disease. WHO. https://www.who.int/emergencies-old/diseases/ebola/frequently-asked-questions
- World Health Organization. (2019a, June). Ebola Virus Disease in Uganda (SitRep #077). WHO | Regional Office for Africa. https://www.afro.who.int/sites/default/files/2019-06/Ebola%20Virus%20Disease%20Sitrep%207%2019th%20June%202019.pdf
- Xinhua. (2018, August 22). Uganda opens Ebola treatment units at border with DRC -– Xinhua | English.news.cn. http://www.xinhuanet.com/english/2018-08/22/c_137410772.htm
- World Health Organization. (2019b, July 3). Ebola virus disease – Republic of Uganda. https://www.who.int/csr/don/13-june-2019-ebola-uganda/en/
- Winsor, M. (2019, June 12). Ebola-stricken boy who became 1st cross-border case in growing outbreak dies. ABC News. https://abcnews.go.com/International/ebola-stricken-boy-1st-cross-border-case-growing/story?id=63656559
- World Health Organization. (2019a, June). Ebola Virus Disease in Uganda (SitRep #077). WHO | Regional Office for Africa. https://www.afro.who.int/sites/default/files/2019-06/Ebola%20Virus%20Disease%20Sitrep%207%2019th%20June%202019.pdf
- World Health Organization, The Republic of Uganda Ministry of Health. (2019, July 25). Weekly Travel Advisory on Ebola virus disease in Uganda [press release]. https://web.archive.org/web/20190725154722/https://health.go.ug/download/file/fid/2349
- Miles, T. (2019, July 19). WHO says investigators conclude Ebola victim did not enter Rwanda. Reuters. https://www.reuters.com/article/us-health-ebola/who-says-investigators-conclude-ebola-victim-did-not-enter-rwanda-idUSKCN1UE1CX
- The Republic of Uganda Ministry of Health. (2019, September 29). Confirmation of an Imported Ebola Virus Disease Case in Kasese District [Press release]. https://reliefweb.int/sites/reliefweb.int/files/resources/29%20August-%20Press%20Release.pdf
