In-depth
Mask mandate effectiveness
There are many examples of the role of policy in facilitating the adoption of new healthy behaviors, from regulations mandating seat-belt use to wearing bicycle helmets to limits on tobacco and alcohol access, use, and advertising. Such policies have historically been met with resistance, often on the grounds of infringement on personal autonomy. However, over time, these have become normalized behaviors for the majority, in part due to mandates, and also because they save lives. In April 2020, some jurisdictions in the U.S. began to implement mandates for community masking as part of a larger strategy to control the COVID-19 pandemic. These mandates were initially put in place with the precautionary principle in mind that the “lack of scientific certainty must not be used as a reason to ignore or postpone preventive or remedial action when there are other good reasons to do so.” Now, there is growing evidence from the jurisdictions where mask mandates are in place that they are effective in reducing COVID-19. This is especially true when additional steps such as fair enforcement, provision of free or affordable masks and a scientific foundation are part of the mandates.
The use of masks and face coverings reduces transmission of SARS-CoV-2, the virus that causes COVID-19. A summary of evidence supporting this is included in the Resolve to Save Lives Mask Guidance Playbook. Masks reduce transmission of SARS-CoV-2 from infected people, whether they have symptoms or not, and whether this transmission is by droplet or smaller aerosol particles. There is growing evidence that masks may also protect wearers by preventing infection, and also possibly by reducing disease severity, as reviewed in last week’s Science Review. Early in the COVID-19 pandemic, there were calls in the U.S. for universal masking of the general public as a means of reducing transmission. In some sectors, such as in health care settings, adoption of universal masking policies occurred sooner than others. Early experience showed signs of benefit, as was described in a Boston hospital where health care personnel as well as patients were required to wear masks. Universal mask wearing was associated with a linear decrease in infections and test positivity rate. However, the U.S. as a nation has largely lacked a unified approach to COVID-19, leaving other sectors, schools, counties and states with fragmented policies and procedures.
Gradually, as evidence mounted supporting the benefits of masking for individuals and communities, more jurisdictions enacted mask mandates. This led to a sort of “natural experiment” in the U.S., enabling us to evaluate the effectiveness of these mandates beyond what models had already demonstrated: mask mandates may have a major impact on the pandemic and save thousands of lives. Models show that the impact of masks is greater as more people wear them, greatest when combined with other public health and social measures, and that even lower-quality masks such as cloth masks could have a major impact. Wei Lyu and George Wehby, both from the University of Iowa, performed a series of analyses to determine how statewide mask mandates affected the growth of COVID-19 cases by looking at how mask mandates related temporally to changes in COVID-19 infections. They showed a compounding decrease in the growth of COVID-19 cases in the 15 states plus Washington, D.C. where community mask mandates were enacted between April 8 and May 15, 2020, after accounting for multiple other factors that could affect changes in transmission dynamics. They estimated that between 230,000 and 450,000 cases of COVID-19 may have been averted by May 22 in states where community mask mandates were in effect. States with mandates in place had less growth in COVID-19 cases than those without mandates. This effect grew over time as mask mandates remained in effect.
Authors’ analysis of US county-level COVID-19 case data between March 31 and May 22, 2020. NOTES Event study estimates (dots) and 95% confidence intervals (bars) of the effects of states mandating community use of face covers or masks when people are in public on the county-level daily growth rate of COVID-19 cases over different periods before and after the mandate order was signed. The reference period was the first five days before the mandate order was signed. The model controlled for major COVID-19 mitigation policies as time-varying (closure of K–12 schools, county-level or statewide shelter-in-place orders, nonessential business closure, closure of restaurants for dining in, closure of gyms or movie theaters), COVID-19 tests per 100,000 people, county fixed effects, and day fixed effects. The model was estimated by least squares weighted by the county 2019 population, and the standard errors were robust to heteroscedasticity and clustered at the state level.
By the end of July, 32 of 50 states (64%) in the U.S. had some version of a mask mandate in place. (The 18 states that had yet to mandate mask use were all led by Republican governors, reflecting politicization of mask policies and mask wearing.) In those states, local mandates were put in place by some mayors. As of Oct. 1, 33 states, Puerto Rico and Washington, D.C. had mask mandates in place. On Sept. 30, Mississippi lifted its mandate, becoming the first state to do so. In general, the mandates require people over a certain age to wear masks when in indoor public settings, on public transportation or when using a rideshare, and in outdoor public settings when physical distancing of 6 feet or more is not possible.
Global studies have also found an association between community masking mandates and improved COVID-19 outcomes. In one preprint study, multivariable analysis was done looking at COVID-19 mortality in 196 countries as it related to various factors such as economics, temperature, population characteristics and early adoption of mask use. In some East Asian countries where mask use was already a cultural norm, and in places where mask use was recommended or mandated by the national government within 30 days of the first case in the country, deaths per million population from COVID-19 were significantly lower. Other factors related to lower mortality were: a greater proportion of the country being under 60 years old; lower obesity rates; less urbanization; and travel restrictions.
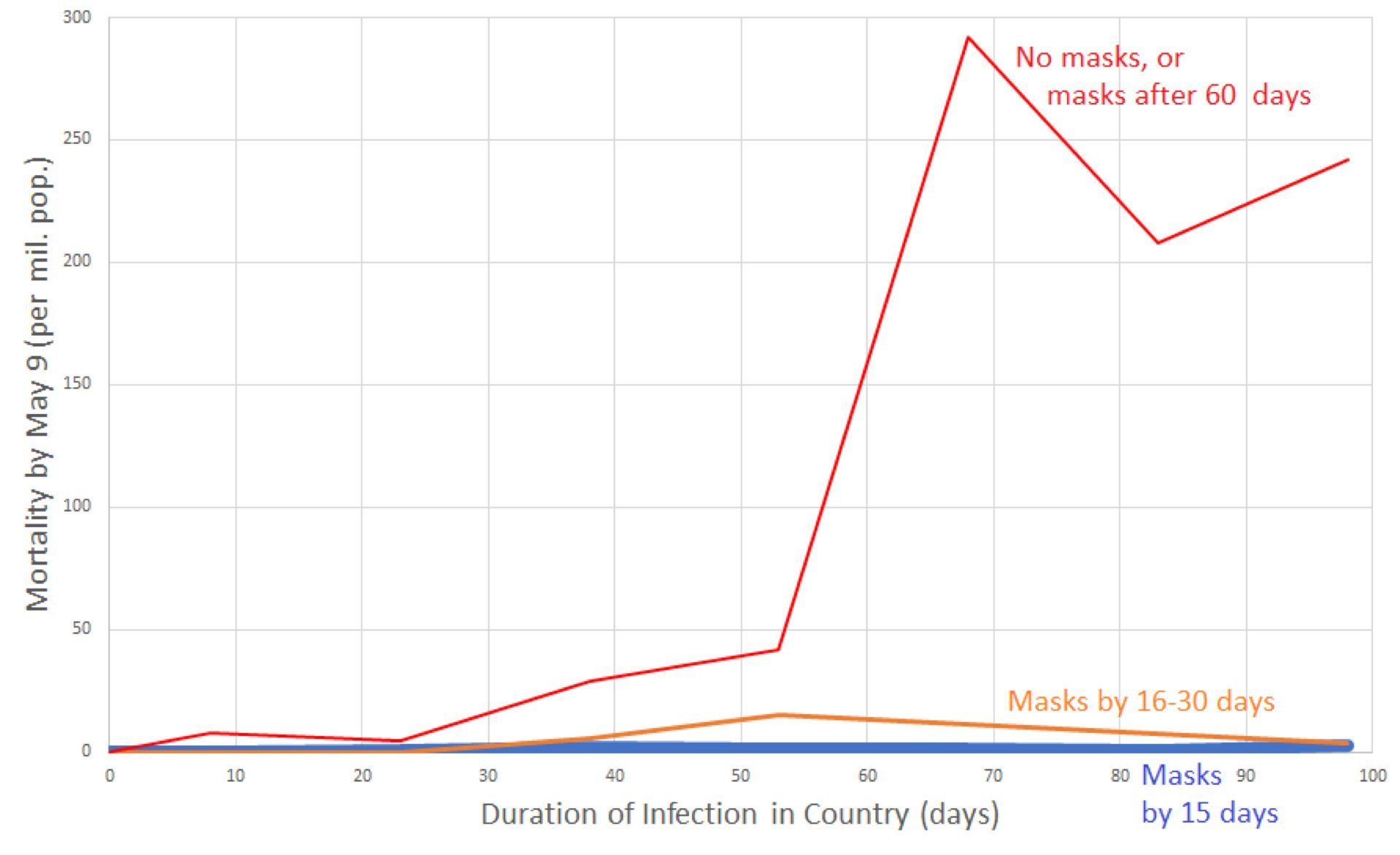
Data grouped by whether country did not recommend masks by April 16, 2020 or recommended them more than 60 days after outbreak onset (red line); recommended masks 16 to 30 days after onset of the country’s outbreak (orange line); or recommended masks (or traditionally used masks) within 15 days of the outbreak onset (blue line close to the x-axis). Country mortality was averaged for the following country groups of infection duration: 0-15 days, 16-30 days, 31-45 days, 46-60 days, 61-75 days, 76-90 days, 91- 105 days. For instance, per-capita mortality for all non-mask or late-masking countries with infection duration between 61 and 75 days was averaged, and graphed at the x-value 68 days. Data for graph derived from 200 countries.
Enacting mandates may not be enough, as is the case with any policy. There needs to be clear and concise communication about any new regulation, and the mandates need to be enforceable. In a recent article published in JAMA, Lawrence Gostin, a professor of public health law, and colleagues address the patchwork that has resulted from the fact that masks are not required in many parts of the U.S., and the variation among the existing mandates. He cautions against a federal mask policy that may be met with legal challenges and may embolden political opposition. Instead, he argues that states should remain key decision-makers in public health and retain autonomy, and that states continue to be better suited to enforce policies, but they need cohesive national direction, guidance, and funding from the Centers for Disease Control and Prevention (CDC). Unfortunately, the relationship between the CDC and state and local public health departments has been challenging during these unprecedented times. Similarly, in their piece titled “Mask Mandates: A Public Health Framework for Enforcement,” Rebekah Gee and Vin Gupta support a national standard based on existing mechanisms in public health and encourage policymakers to push for enforcement policies within a national directive.
Despite the patchwork of policies, there are indications that the local epidemiology of COVID-19 in different parts of the U.S. may be influenced by whether or not a mask mandate is in place. Alabama, Kansas, Oklahoma, South Carolina and Texas are just some of the states that have reported differences in COVID-19 case counts, emergency room visits for COVID-like illness, hospitalizations due to COVID-19, COVID-19-related death counts, and/or test positivity rates among locales with mask mandates and those without. These reports did not rigorously address the potential influence of factors other than mask mandates, including the effects of other mitigation measures, that may accompany mask mandates. In addition, there may be differences between locales in terms of risk of COVID-19 spread and severe disease because of population density, population demographics and other factors such as access to health care. Lastly, implementation of a mandate does not assure that people will follow it. Monitoring mask use is an essential component of an effective public health approach to COVID-19 and should be included in a comprehensive program to increase mask use as part of an overarching strategy to control the virus. Our list of 15 essential indicators required for an effective COVID-19 response includes mask use surveillance, and Hawaii and Utah have recently included mask compliance data in their state COVID-19 dashboards.
A recent report on the trends in COVID-19 incidence in Arizona after implementation of mitigation measures examines the impact of mitigation measures on SARS-CoV-2 transmission. Authors assessed the relationship between the number of COVID-19 cases relative to implementation of enhanced community mitigation measures. In June, the average number of daily cases in Arizona increased dramatically after the stay-at-home order was lifted. On June 17, local officials began implementing and enforcing mask-wearing via county and city mandates, affecting approximately 85% of the state population. Statewide mitigation measures, such as promotion of social distancing, limits on large gatherings, and closures of certain businesses, were also put into place. The number of COVID-19 cases in Arizona peaked during June 29–July 2, stabilized during July 3–July 12, and further declined by approximately 75% during July 13–August 7. Although it was not possible to distinguish the effects of mask mandates from the effects of other mitigation measures, the implication of these findings is that widespread implementation of community mitigation measures including mask-wearing can reduce transmission of SARS-CoV-2.
In a study that estimated the effects of mask mandates on the transmission of SARS-CoV-2 in Canada, authors assessed mask mandates separately from other mitigation measures. Mask mandates were implemented in a staggered fashion across Ontario’s 34 public health regions while province-level policies were held constant, and similar staggerings of mitigation measures were observed across Canada as a whole. Authors estimated that mask mandates were associated with an average reduction of 25% to 31% in the weekly rolling average of COVID-19 cases in Ontario and with a 36% to 46% average reduction in weekly cases across Canada, independent of the effects of other mitigation measures. Authors also reported a correlation between mask mandates and increased mask use, assessed by self-report surveys administered across Canada.
When recommendations for universal masking were made early in the pandemic, they were made with the precautionary principle in mind: that a low-cost, low-risk intervention that has the potential to save lives should be adopted, even if the empiric evidence for it is not yet complete, while evidence-gathering continues. As more was learned about COVID-19, it became clear that increased mask use could substantially reduce spread of the virus. Increasing evidence from the U.S. and other countries suggests that mandates increase mask-wearing and thereby reduce spread of the virus. Enforceable mask mandates should be a part of a package of mitigation strategies to address the ongoing COVID-19 pandemic.
Weekly Research Highlights
Note: U.S. CDC also publishes a COVID-19 Science Update
COVID-19 Transmission in the U.S. Before vs. After Relaxation of Statewide Social Distancing Measures
(Clinical Infectious Diseases, Oct. 3, 2020)
- The researchers used Rt (the estimated number of people infected by each infected person) as the outcome variable. Rt was estimated based on deaths due to COVID-19 rather than cases to avoid biases in case detection due to the amount of testing as well as testing turnaround time.
- All 51 jurisdictions implemented at least one public health and social measure. Median time to relaxing at least one measure was 47 days, with easing of work restrictions usually the first measure relaxed (40 states) followed by reopening service industry establishments (32 states).
- 44 jurisdictions achieved an average decline in Rt over time while restrictions were in place, with all but five reaching an Rt <1 before relaxing restrictions.
- Four states (Alaska, New York, South Dakota and Tennessee) maintained a downward trajectory in their Rt in the eight weeks after relaxing restrictions and eight kept Rt under 1. (Note: the four states have not been able to sustain this reduction, and at the time of writing South Dakota had the highest rate of COVID-19 in the nation). States with more severe epidemics before relaxation saw a lower increase in Rt after relaxation of measures, potentially due to continued social distancing despite relaxation of measures.
- Limitations of the study include the fact that Rt is based primarily on deaths, which may not represent transmission as infection fatality rates have declined over time and differ based on age and other factors, and completeness of death reporting varies among jurisdictions. Also, the study is observational and the associations seen between Rt and relaxation of restrictions may not be causal.
Survival of SARS-CoV-2 and Influenza Virus on the Human Skin: Importance of Hand Hygiene in COVID-19
(Clinical Infectious Diseases, Oct. 3, 2020)
- SARS-COV-2 survival time was approximately eight times longer than flu virus on all tested surfaces (metal: 84 v. 12 hours; glass: 85 v. 11 hours; plastic: 58 v. 6 hours).
- Investigators tested virus survival in both a culture medium and in mucus to see if the virus-inactivation properties of mucus operated similarly on both viruses. While the flu virus was more rapidly inactivated in a mucus solution compared to a culture medium (except on skin), SARS-COV-2 was similarly stable regardless of the solution.
- To test virus survival on skin, investigators used skin samples recovered from autopsies, as exposing people to SARS-COV-2 would be unethical. They were able to compare their skin samples to skin on live humans using influenza A virus and found no significant difference.
- Limitations of the study include that only a few skin and mucus samples were used (three each) and that this study cannot distinguish between levels of virus that are sufficient to infect someone with either virus and those that are too low to infect someone.
Please note there will be no Weekly Science Review next week. The next one will publish on October 27th.
Suggested citation: Cash-Goldwasser S, Jones SA, Bochner A, Cobb L and Frieden TR. In-Depth COVID-19 Science Review October 3 – 9, 2020. Resolve to Save Lives. 2020 October 13. Available from https://preventepidemics.org/covid19/science/review/