In-Depth
The role of T cells in adaptive immunity to COVID-19
B cells and T cells are both white blood cells that are part of the body’s adaptive immune system, and both play a role in fighting infections. B cells, the main actors in humoral immunity, act by recognizing patterns on the outside of harmful organisms called antigens. They then go through a process of differentiation that releases antibodies to further augment the body’s ability to recognize and fight infection. T cells, the main actors in cell-mediated immunity, act by recognizing cells that are foreign or have become abnormal because of infection; the T cells destroy these cells and then adapt themselves to better recognize and kill similar cells in the future. Both B and T cells have a “memory” component that allows the body to remember a prior infection and protect itself from it or act against it more quickly in a future encounter (protective immunity). While much attention has been given to the body’s humoral immune response to SARS-CoV-2, the virus that causes COVID-19, and the role of B cells and antibodies in protective immunity, more evidence is emerging about the possible role of memory T cells and the body’s cell-mediated immune response to the virus. Specifically, current evidence is suggesting that prior infection with other human coronaviruses may confer some crossover immunity through the action of T cells.
SARS-CoV-2 is the seventh coronavirus known to infect humans. Of the six others, four cause common colds. The other two cause more severe disease: MERS-CoV, the virus that causes Middle Eastern Respiratory Syndrome (MERS, first identified in 2012), and SARS-CoV-1, the virus that causes Severe Acute Respiratory Syndrome (SARS, first identified in 2002). In a recent study published in the journal Nature, the authors demonstrate through laboratory experiments how memory T cells from people previously infected by other human coronaviruses can potentially mediate infection from SARS-CoV-2. They also performed experiments to study the development of SARS-CoV-2-specific memory T cells after recovery from COVID-19, something that has previously been shown to happen after recovery from SARS and MERS. The authors were able to show that plasma from recovered SARS patients who were infected nearly 17 years prior contained memory T cells that cross-reacted in recognizing parts of the SARS-CoV-2 virus. To a lesser degree, they were also able to show cross-reactivity in patients without any history of SARS or COVID-19, possibly due in part to common-cold coronaviruses or animal coronaviruses. This type of cross-reactivity could help explain the spectrum of disease in COVID-19, with asymptomatic or milder infections potentially happening in people with some pre-existing T-cell mediated immunity from other coronavirus infections in the past.
Other studies such as a recent report in Science Immunology highlight the importance of this potentially long-lasting type of T-cell immunity given that much of the research increasingly shows that B-cell and antibody responses to COVID-19 produce relatively short-lived protection, if any. B and T cells often work together as part of building and mounting an immune response, however, in some types of infections, one can play a more dominant role than the other, especially in establishing long-lasting protection from reinfection. It is possible, for example, that mild infections may not be severe enough to result in a productive B -cell and antibody response, yet could still be able to produce a T-cell response and memory, a possibility that is raised in the Science Immunology report. In addition, a preprint study examining discordant humoral and cell-mediated response was able to show that some people developed evidence of T-cell immunity without seroconversion, that is, without developing antibodies.
Currently, there is growing evidence that T cells from prior coronavirus infections do cross-react with SARS-CoV-2. However, it has yet to be determined to what degree this would account for differences in susceptibility and severity of disease in patients. Although antibody protection, if any, may wane within months after COVID-19 infection, memory T cells may continue to offer long-lasting protection against reinfection. Other recent studies have also tried to address the different levels of severity among people with COVID-19 by showing evidence of existing T-cell cross-reactivity to SARS-CoV-2 in human blood samples drawn before the virus was identified. To date, there is no direct human evidence to determine the practical implications of these lab findings.
Seasonal influenza during the COVID-19 pandemic
At the start of the COVID-19 pandemic, many public figures compared the new disease to the flu. Both are spread in similar ways, both are caused by RNA viruses, and the clinical illnesses that most infected people experience can be hard to tell apart. Some of these comparisons may have led people to underestimate the novel coronavirus. Over the past months, we have learned that COVID-19 is transmitted far more easily and is more likely to cause serious and fatal illness than the seasonal influenza many people are familiar with. Although both diseases can occur throughout the year, and in all sorts of climates, SARS-CoV-2, the virus that causes COVID-19 and influenza viruses can spread more easily under cool and dry conditions. Some public health experts have warned that health systems in North America and Europe will face a double challenge if the coming fall and winter weather fuels both another wave of COVID-19 and the usual seasonal influenza epidemics. As well as the additional stress on health systems, people who get both infections back to back or at the same time may face added health risks.
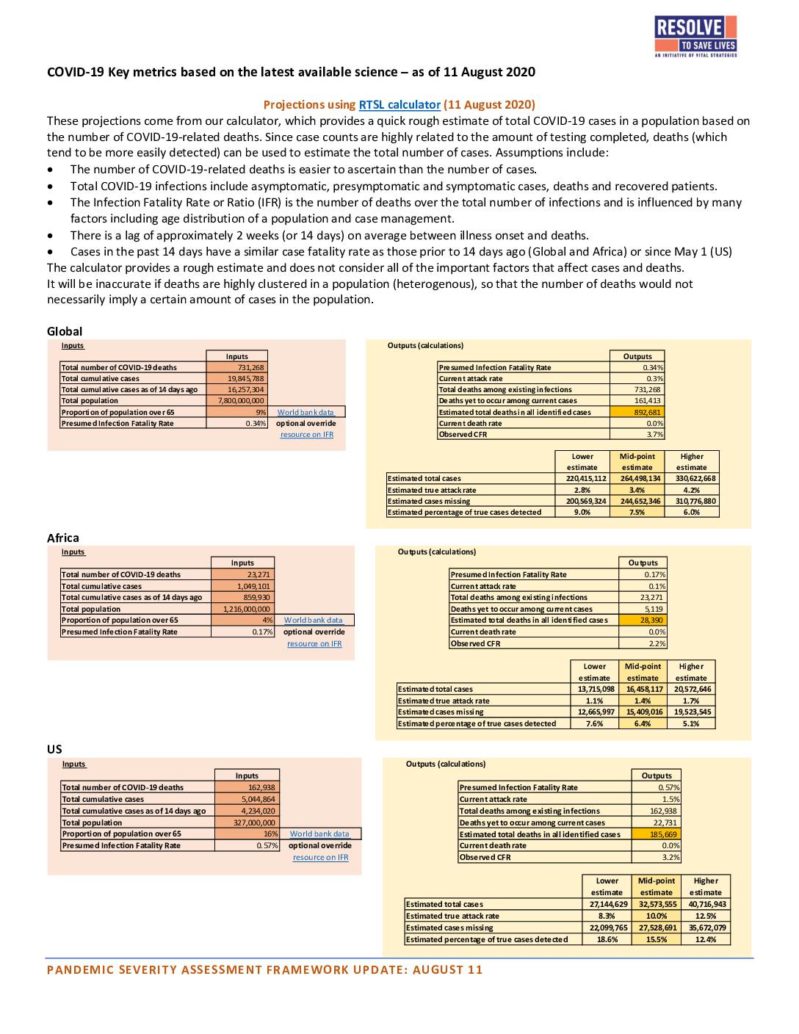
Fortunately, the same public health and social measures that have been recommended to curtail COVID-19 also work exceptionally well to reduce influenza and some other respiratory infections. In an earlier Weekly Science Review, we presented flu surveillance data from countries that were affected by COVID-19 in March and April. After implementing COVID-19 responses, including mandated restrictions, many saw their influenza cases drop off weeks earlier than expected. In temperate countries of the Southern Hemisphere seasonal influenza usually occurs from May to September. In its most recent surveillance update, the World Health Organization (WHO) concludes that the Southern Hemisphere’s 2020 flu season hadn’t even started as of July 19, right when many countries expect to see case counts cresting. The image below shows seasonal influenza cases experienced in Chile for the first 28 weeks of each year since 2015, with barely any activity in 2020. Even in tropical countries where flu can occur sporadically year-round, influenza cases and positive samples reported to WHO have been sparse in recent weeks, and none at all were reported from tropical zones of Africa, South America, or Southeast Asia.

This may be an encouraging trend, if it truly reflects that efforts to mitigate or suppress COVID-19 are simultaneously reducing the burden of another potentially grave respiratory illness such as seasonal influenza. Furthermore, with less global travel, there may be less global circulation of influenza viruses. WHO warns, however, that at least part of what’s being observed may be a collateral effect of the COVID-19 pandemic. If fear or mandated restrictions deter many people from seeking treatment, influenza cases may go undetected and unreported. If hospitals and health systems are overburdened with COVID-19, they may not be able to test and report on influenza as effectively as they have in prior years. And there is another reason for those of us in the Northern Hemisphere to be concerned: each year epidemiologists and virologists monitor seasonal influenza in the south in order to anticipate the coming season in the north (and they learn from what happens in the north to anticipate the following season in the south). That includes important work to select viruses for the seasonal flu vaccine and to anticipate how extensive transmission is likely to be. With so little seasonal transmission happening now, it will be harder to prepare for the Northern Hemisphere flu season in the coming months and predict which strains are likely to circulate, if there is a widespread influenza season. For their part, vaccine manufacturers are gearing up to produce and ship record numbers of flu shot doses for the coming season. Ultimately, according to Johns Hopkins University’s Outbreak Observatory, “the severity of seasonal influenza in the Northern Hemisphere may depend heavily on how well countries are containing COVID-19.” Wherever widespread COVID-19 transmission is occurring, seasonal influenza is likely to spread rapidly as well. Wherever health systems are already stressed by COVID-19 cases, the added burden of influenza will compound the crisis. Health officials should prepare to respond to both COVID-19 and seasonal influenza. Some localities will want to strengthen their public health and social measures. In addition, ensuring that seasonal influenza vaccine is widely available may require new approaches for safely delivering it to record numbers of people during the pandemic. For their part, people can protect themselves and prevent the spread of both viruses by continuing to take recommended precautions (masks, distancing, and handwashing) and by getting a flu shot as soon as possible after it becomes available in their area (in September or October in the United States).
Weekly Research Highlights
SARS-CoV-2 Transmission and Infection among Attendees of an Overnight Camp — Georgia, June 2020
(MMWR, Aug. 7)
- An investigation was launched by the Georgia Department of Public Health after a teenage staff member at the overnight camp developed symptoms consistent with COVID-19 on June 23 and subsequently tested positive. All campers and staff were sent home by June 27. As part of its involvement, the health department recommended quarantine and testing of all staff and campers, and isolation as necessary. The camp had begun with a training and orientation session on June 17. The 120 staff members who conducted the orientation stayed on and were joined by 363 campers and three additional staff members on June 21, while 138 trainees returned home on June 20 after the orientation session. By collecting testing information, the health department was able to calculate attack rates among staff/trainees and campers.
- The median camper age was 12 (range 6-19) and the median staff age was 17 (range 14-59). A total of 597 Georgia residents were at the camp from June 17 to June 27 when the camp was closed. Of these, test results were available for 344. Of those tested, 76% had a positive test for an overall attack rate of 44%. Attack rate was highest among staff members (56%) who had been at the camp the longest. When stratified by age, those 6 to 10 years old had the highest attack rate (51%), followed by those 11 to 17 years old (44%) and those 18 to 21 years old (33%). Information of symptoms was available for 138 of those who tested positive and 26% of positive tests were among people with no symptoms.
- Attack rates were likely underestimates of true values given that 42% of attendees were not tested. Individual risk factors and adherence to PHSMs are not known. People may have been exposed to COVID-19 before or after attending the camp.
Risk of COVID-19 Among Front-line Health-Care Workers and the General Community: A Prospective Cohort Study
(Lancet Public Health, July 31)
- Participants who enrolled in a mobile application during March and April 2020 agreed to provide information about COVID-19 illness symptoms and testing results. After an average follow-up period of 35 days, 5,545 participants reported a positive test. The prevalence of COVID-19 was 2,747 cases per 100,000 front-line health care workers compared with 242 cases per 100,000 among other people. After statistically correcting for their higher access to testing, the researchers found that health workers were at least three times more likely to develop COVID-19 (aHR=3.40, 95% CI 3.37–3.43).
- Health workers who said they had adequate PPE were at lower risk of testing positive than their colleagues who relied on reused or inadequate PPE. The analysis also showed that Black, Asian and minority ethnic health workers were more likely to become infected than their white co-workers. The highest rate of infection was observed among health care workers in inpatient settings.
- This large prospective study quantifies the considerable additional risk for COVID-19 that front-line health workers faced earlier this year in the U.K. and U.S. Although the study design, analytic methods and very large sample size inspire confidence in the findings, there remain some potential biases and limitations. The non-representative sample was overwhelmingly recruited in the U.K., and depended on people being willing to enroll and use the application during a relatively short period of time fairly early in the pandemic. Infection risks may differ in other countries, among people who are uninterested or unable to access the app, at different stages of their local epidemics, or as community and health facility prevention strategies adapt to new information about how to control COVID-19.
Hospitalization Rates and Characteristics of Children Aged <18 Years Hospitalized with Laboratory-Confirmed COVID-19 — COVID-NET, 14 States, March 1–July 25, 2020
(MMWR, early release Aug. 7)
- To better understand factors among children being hospitalized for COVID-19, researchers queried the COVID-NET surveillance system to characterize hospitalizations among those under 18 years old. COVID-NET collects information about COVID-19-associated hospitalizations from 14 states. The researchers looked at: demographic information such as age, sex and race; underlying medical conditions; and information about the hospitalization such as duration, treatments and level of care required.
- From March 1 to July 25, 576 children hospitalized with COVID-19 were reported to COVID-NET. The cumulative COVID-19 hospitalization rate for children during this period was eight per 100,000 compared to 164.5 per 100,000 for adults. Infants under 3 months old accounted for almost 20% of all hospitalizations in children. The median age was 8 years old, and close to evenly split between males and females. Latinos accounted for 46% of the hospitalizations, followed by Blacks at 30% and whites at 14%. Information on underlying medical conditions was available for 38% of the hospitalized children and among those, 42% had one or more underlying medical conditions. One-third of the children required ICU admission for a median of two days. Among 208 hospitalizations for which disposition was known, there was only one reported death.
- Most of the pediatric cases submitted to COVID-NET had not had a chart review, raising the possibility of bias among those that had. Comprehensive information about multisystem inflammatory shock syndrome in children (MIS-C) is currently not available from COVID-NET.
Suggested citation: Cash-Goldwasser S, Kardooni S, Cobb L, Bochner A, Bradford E and Shahpar C. In-Depth COVID-19 Science Review August 1 – 7, 2020. Resolve to Save Lives. 2020 August 11. Available from https://preventepidemics.org/covid19/science/review/