Update: Opening K-12 schools for in-person learning amidst vaccines and variants: what have we learned and how can this guide us?
What factors may explain recent trends in cases and hospitalizations among school-aged children?
Cases
Case rates have risen among all age groups. However, in recent weeks, the number of new cases has risen particularly among children under 18 years old, who now comprise a higher proportion of new cases than previously. According to data from the CDC, among 38 million COVID-19 cases reported in the U.S. since the pandemic started, approximately 13% of those (3.8 million) were in children under the age of 18. However, data compiled by the American Academy of Pediatrics indicated that for the week of August 19-26, 22% of all reported COVID-19 cases were in children. There has been a 24-fold increase in the number of COVID-19 cases reported among children in the past nine weeks (June 24 to August 26).
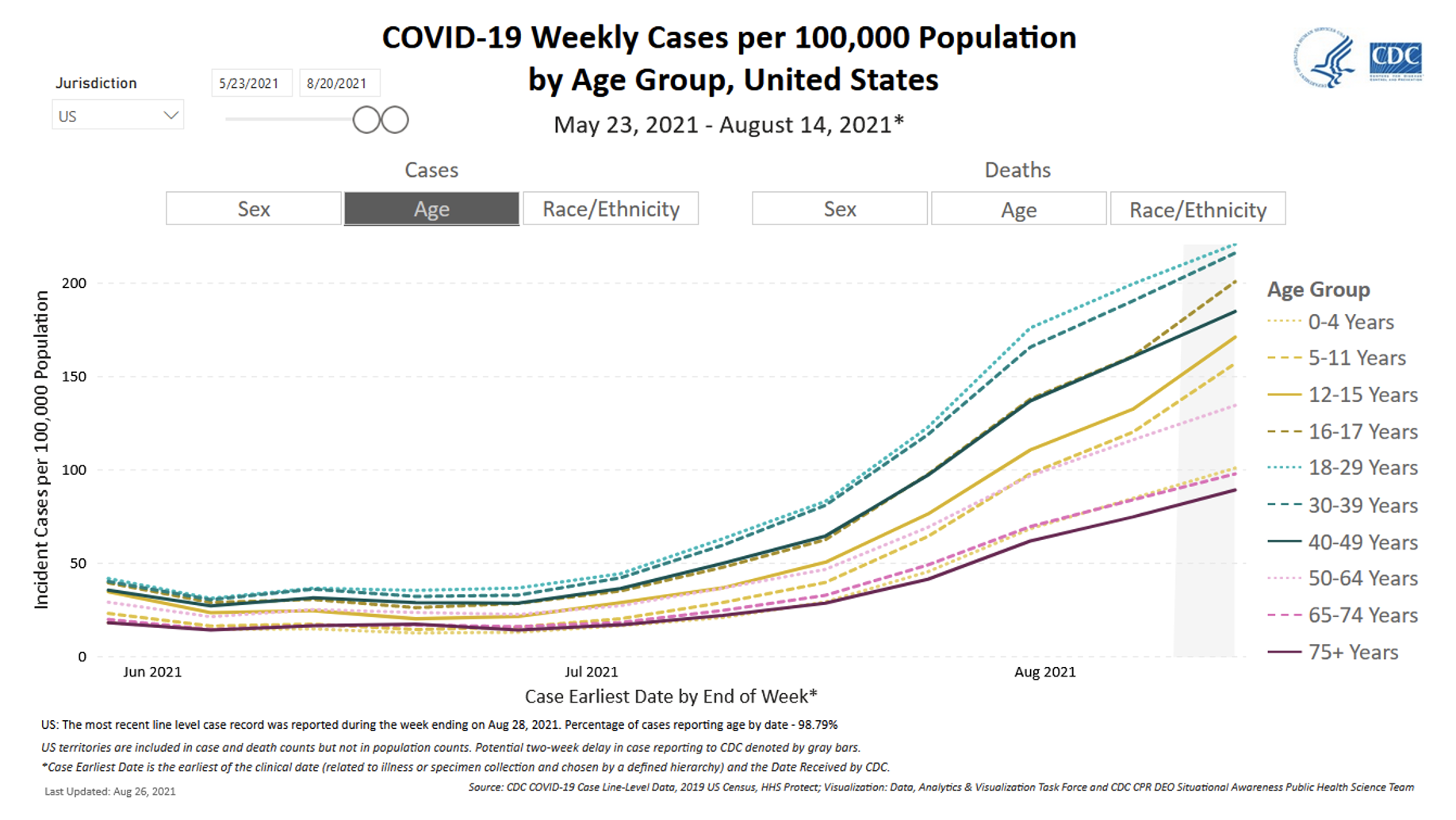
Source: CDC
The increased transmissibility of the Delta variant is contributing to the rapid increase in COVID-19 transmission observed in the U.S. over the past two months, including among children. Whereas fewer than 10% of cases in the U.S. were caused by the Delta variant in May 2021, the Delta variant now accounts for more than 98% of U.S. cases. In an analysis of 1.7 million SARS-CoV-2 sequences uploaded to the Global Initiative on Sharing All Influenza Data (GISAID) database from 64 countries, the Delta variant approximately twice as transmissible as the original virus. Estimates like these suggest that the Delta variant is about as contagious as the virus that causes chickenpox. Factors that may contribute to Delta’s increased transmissibility include high viral loads (amount of virus present during infection) and a fast viral replication rate that makes it possible to transmit the virus earlier in the course of infection.
There is no evidence that the increase in Delta’s transmission rate puts children at greater risk than adults; in fact, as we previously wrote, children may still be at lower risk of acquiring and transmitting SARS-CoV-2 infection than adults. Rather, the relative increase in COVID-19 cases among children may simply reflect how a nationwide surge in cases is impacting the least-vaccinated segment of the population. There are 50 million Americans (14.4% of the total population) under age 12 who are not yet eligible to be vaccinated. In addition, vaccination rates remain low among adolescents: only 34% of those aged 12-15 and 44% of those aged 16–17 are fully vaccinated, compared to 63% of adults aged 18 or older.
Other factors likely contributing to this surge include the relaxation of public health and social measures such as masking requirements, capacity limits in indoor public spaces and closures of high-risk settings, which had previously helped to limit close contact and mitigate the spread of COVID-19.
Hospitalizations
With the surge in cases has come a rise in hospitalizations. Currently, about 12,000 people per day, including about 300 children, are admitted to the hospital with COVID-19 nationwide. While this is less than the January 2021 peak of more than 16,000 new daily admissions, the number of new admissions increased rapidly during August. New admissions of patients with confirmed COVID-19 are currently at their highest levels since the start of the pandemic in Alabama, Florida, Louisiana, Mississippi, Oregon and Washington. The number of new hospital admissions among young people under age 18 is now at the highest level observed during the pandemic. However, older age is a major risk factor for severe COVID-19, and children still make up a small proportion of the total number of people hospitalized with COVID-19. According to reporting from the American Academy of Pediatrics, children currently make up only 2-4% of patients hospitalized with COVID-19, a percentage that has been relatively steady throughout the pandemic.

Source: CDC Data Tracker
Is Delta causing more severe illness in children than earlier variants?
The rising numbers of hospitalizations have raised questions about whether the Delta variant is causing more severe illness in children. As outlined in a recent article, anecdotally, doctors are reporting that some children are appearing at hospitals sicker and deteriorating faster than at earlier points in the pandemic. However, we still do not have robust scientific evidence that Delta is causing more severe illness in children or adolescents specifically.
There is some evidence that Delta may cause more severe illness. For example, a recent study that analyzed data from England on over 40,000 COVID-19 cases of all ages showed that among unvaccinated people, those with the Delta variant were at higher risk of hospitalization than those with the Alpha variant. A study from Singapore that compared outcomes among hospitalized COVID-19 patients of all ages with Delta to outcomes among hospitalized COVID-19 patients with the original virus strain found that Delta was associated with a significantly higher risk of poor outcomes (needing oxygen, requiring admission to the intensive care unit, or death). Comparisons across time and groups of patients can be confounded by baseline differences between study populations and by changes in what we have learned about how to treat COVID-19; more data are needed to determine the extent to which Delta may increase risk of severe disease, including for specific populations such as children.
What do we know about COVID-19 Vaccines and the Delta variant?
Recent data from the U.S. have shown that vaccine effectiveness against severe disease caused by Delta remains high, although effectiveness against infection has fallen to some degree. For example, data reported to CDC from approximately 15,000 skilled nursing facilities or nursing homes from March 1 to August 1, 2021, showed that during the pre-Delta period, vaccine effectiveness against infection was 74.7% for Pfizer and Moderna vaccines, whereas during the period when Delta was the most common variant, vaccine effectiveness against infection was 53.1% for Pfizer and Moderna vaccines. A study that analyzed data on SARS-CoV-2 infections and vaccinations from adults living in New York State between May 3 – July 25, 2021 found that vaccine effectiveness against infection declined from 92% to 80% over the course of the study, while vaccine effectiveness against hospitalization remained stable (92-95%). Whether declines in effectiveness against infection are due to immunity waning over time or to the prevalence of the Delta variant is challenging to determine, as these events are occurring concurrently.
When vaccinated people do become infected, these breakthrough COVID-19 infections tend to be milder than infections among unvaccinated people. However, we are still learning about the risk of onward transmission from Delta breakthrough infections.
Recent evidence suggests that transmission from breakthrough infections is possible. A study of a COVID-19 outbreak linked to large public gatherings in Barnstable County, Massachusetts found that the amount of SARS-CoV-2 virus detected in diagnostic samples did not differ between breakthrough cases and unvaccinated cases. This study did not assess whether detected virus was viable (capable of causing infection) or quantify rates of onward transmission, and samples were from people who opted to be tested, which may have excluded mild or asymptomatic infections. To determine the risk of transmission associated with breakthrough infections, further studies including real-world data on transmission patterns are needed.
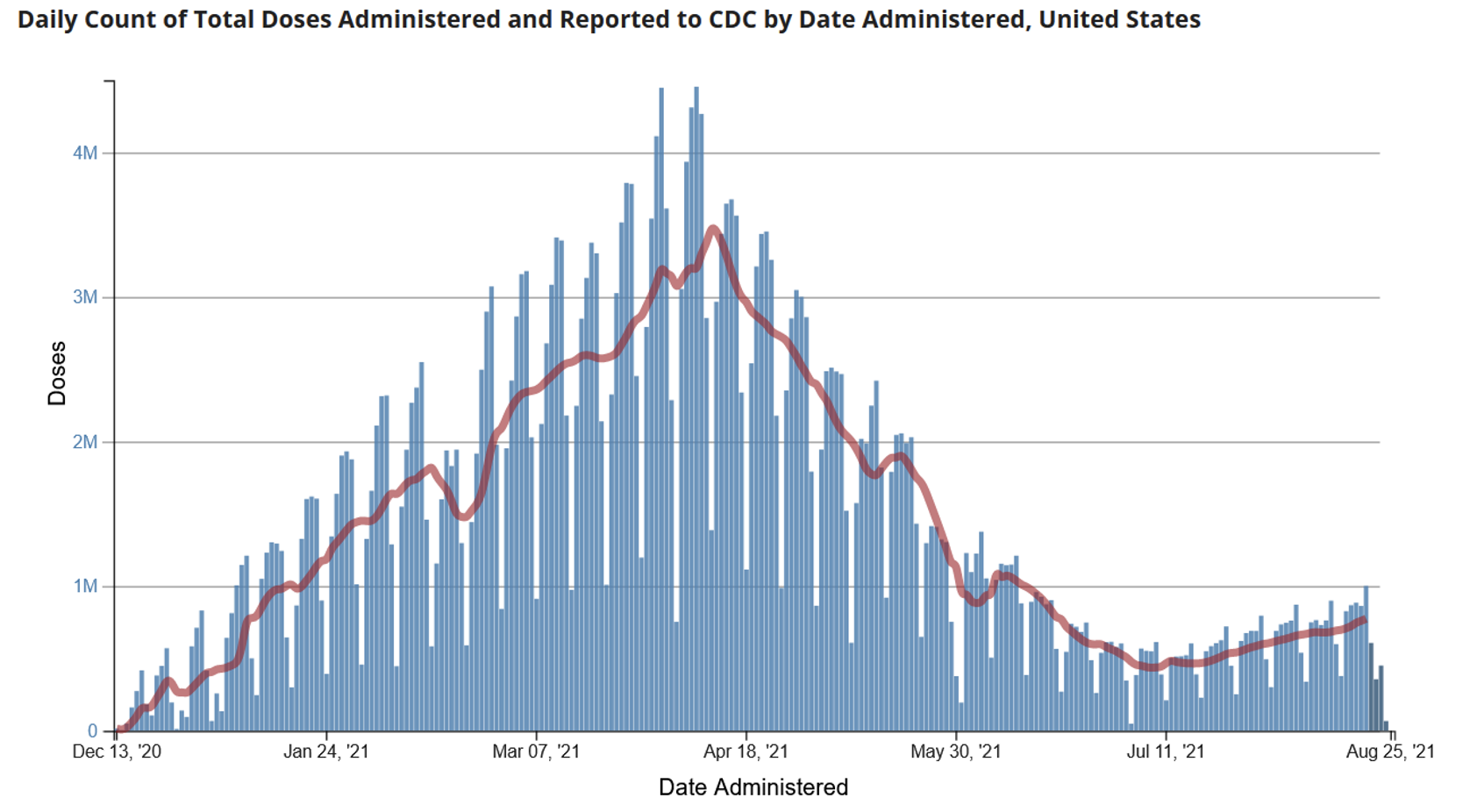
Source: CDC
How have high community transmission rates affected schools?
High rates of community transmission have resulted in a challenging start to the school year in some districts. Media reports suggest that tens of thousands of children are under quarantine due to COVID-19 exposures and some schools have had to postpone in-person education due to the number of cases among students or staff and resulting staff shortages. For example, 20,000 students—nearly 5% of the Mississippi state public school population—were reported to be in quarantine because 800 students tested positive during August 2-6. In Georgia, because of the rapid increase in cases among school-aged children, 68,000 students have been affected by closures of school districts for in-person learning.
What can be done to reduce the spread of COVID-19 in schools?
In a recent review, we identified abundant evidence on how the risk of transmission and outbreaks in schools can be reduced using layered mitigation measures. Per recent CDC guidance for COVID-19 prevention in K-12 schools, key mitigation measures include:
- Vaccination for everyone who is eligible
- Universal, consistent and correct mask use
- Ventilation
- Physical distancing
- Screening testing and contact tracing to promptly identify cases, clusters and outbreaks
- Handwashing and respiratory etiquette
- Staying home when sick and getting tested
- Cleaning and disinfection
A new analysis of Los Angeles County data adds to existing evidence that schools that implement layered prevention measures can keep students and staff relatively safe from COVID-19 even when community transmission rates are high. Researchers compared COVID-19 case rates among students and staff who attended Los Angeles County schools—which implemented prevention measures such as symptom screening, masking, physical distancing and cohorting—to case rates in the broader community between September 2020 and March 2021. Results showed that the rate of school-associated cases among students attending school in-person (kindergarten – 12th grade) remained low, and that the rate of COVID-19 cases not associated with in-school transmission was higher among children in the same age group living in Los Angeles County. School-associated case rates among staff members were also generally lower than case rates among adults in the county.
Two recent studies further highlight the importance of vaccination among school staff to prevent SARS-CoV-2 infections. The School District of Philadelphia—one of the nation’s largest school districts—reopened for in-person instruction the week of March 21, 2021, with required weekly SARS-CoV-2 testing for all employees. During the initial five weeks after schools reopened, 34,048 tests were performed, 0.7% of which returned a positive result. Fully vaccinated employees (reporting two vaccines doses) were 95% less likely to test positive for COVID than unvaccinated employees (0.09% vs 1.76% testing positive overall).
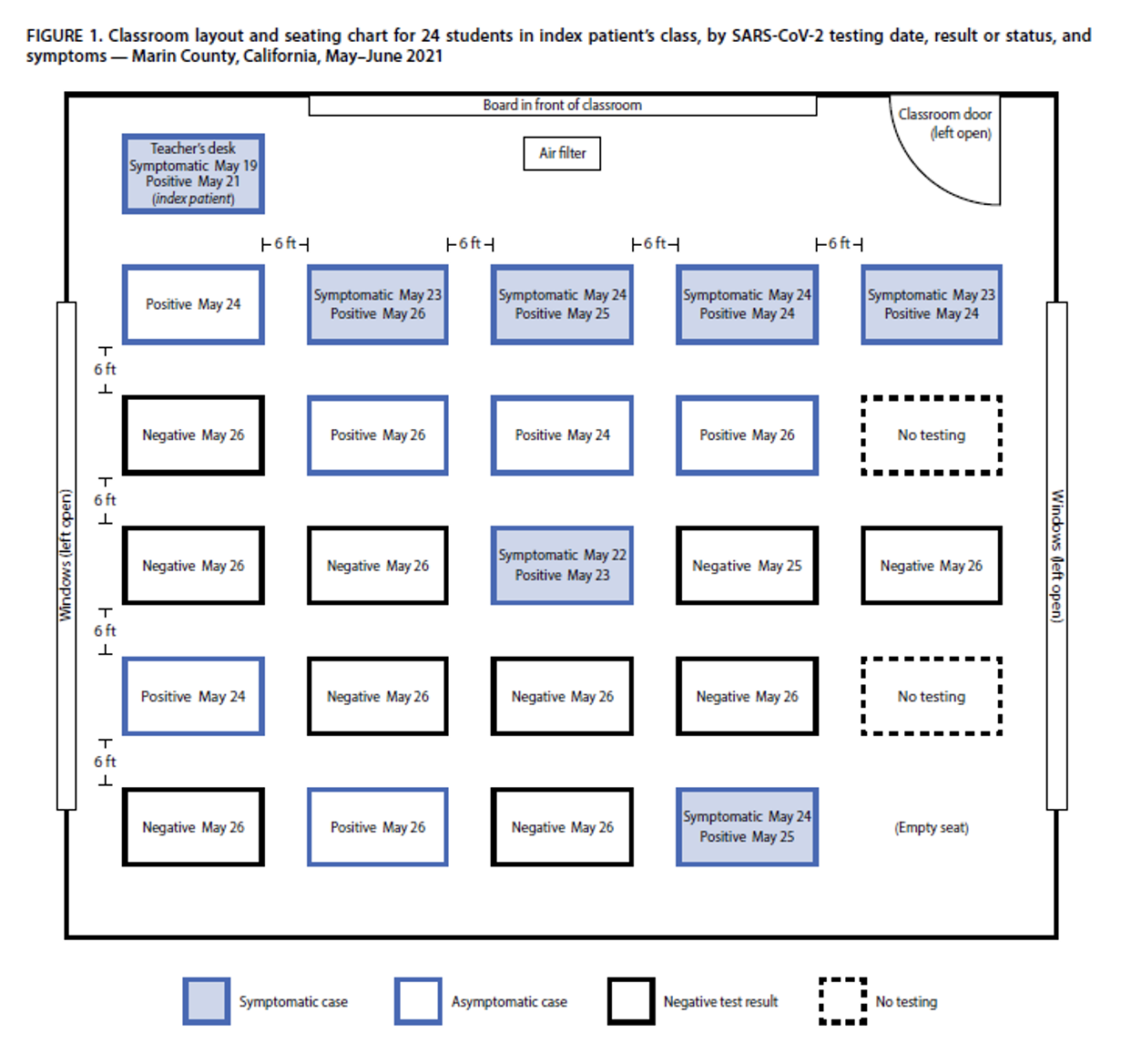
In May-June 2021 in Marin County, California, an unvaccinated teacher worked for two days while symptomatic from COVID-19 caused by the Delta variant. The teacher unmasked to read aloud to the class. Twelve of the 24 students in the teacher’s class were infected; the outbreak ultimately led to a total of 26 cases among school students and their families. Students infected during the outbreak were too young to be eligible for vaccination. Layered mitigation measures, including masking, distancing and increased ventilation were in place and likely limited the scope of onward transmission in the school, but this outbreak reinforces the importance of vaccination among school staff working with students who are not yet eligible to be vaccinated.
In-person learning is critical for the health of children and their communities, and we must do everything we can to keep our children and communities safe from COVID-19. A key step towards protecting in-person learning is to control community transmission because high community case rates are linked to an increased risk of transmission and outbreaks in schools. Increasing vaccination coverage among all eligible persons is the most effective way to lower community transmission. While working to increase vaccination coverage, communities with high rates of transmission can implement public health and social measures shown to reduce transmission, such as masking, physical distancing, and avoiding large in-person gatherings. In all communities, we must implement and consistently practice layered mitigation measures in schools in order to protect students and staff from COVID-19.
Suggested citation: Cash-Goldwasser S and Jones SA. In-Depth COVID-19 Science Review September 1, 2021. Resolve to Save Lives. 2021 September 1. Available from https://preventepidemics.org/covid19/science/review/