In-Depth
Declining death rates among people severely ill with COVID-19
By the end of October, daily COVID-19 cases in the United States reached a record high, yet daily deaths remained far less than the peak that occured in April. Although some of this is due to a lag in deaths, during July, COVID-19 hospitalizations in the United States reached similar levels to April, but deaths remained far below April’s numbers. Beyond the United States, case fatality rates declined in 43 countries between the first and second peaks of COVID-19 cases.
Of the many possible reasons for this decline in mortality—one that received a lot of attention—was the change in the age distribution of those infected. For instance, in the United States, the median age of confirmed cases declined from over 45 years old at the beginning of May to under 40 years old throughout July and August. The age group with the highest incidence changed from those over 80 to those 20 to 29. Similarly, hospitals in Houston documented lower death rates during the second surge of COVID-19 cases compared to the first (5% versus 12%); at the same time patients were younger and had fewer comorbidities. Given that infection fatality rate (percentage of people with COVID-19, regardless of diagnosis, who die from the disease) increases with age and comorbidities, these changing dynamics might be enough to explain the change in the case fatality rate (percentage of people diagnosed with COVID-19 who die from the disease).
Recent evidence, however, suggests that improved outcomes among older people infected with COVID-19 may also be driving the decrease in mortality. Dennis et al. examined the changing mortality rates over time among a cohort of over 21,000 critical care patients admitted to hospitals in England between March 1 and the end of June. After controlling for age, sex, comorbidities, ethnicity and region of the county, mortality was highest for patients admitted at the end of March and then declined by 9% per week for intensive care unit patients and 12% per week for other critical care patients (see Figure 1). A study by Horwitz et al. looking at New York University’s hospital system in New York City between March and August saw similar results. Adjusting for age, severity of COVID-19 on admission, and comorbidities, mortality among those hospitalized decreased from 26% in March to 8% in August.
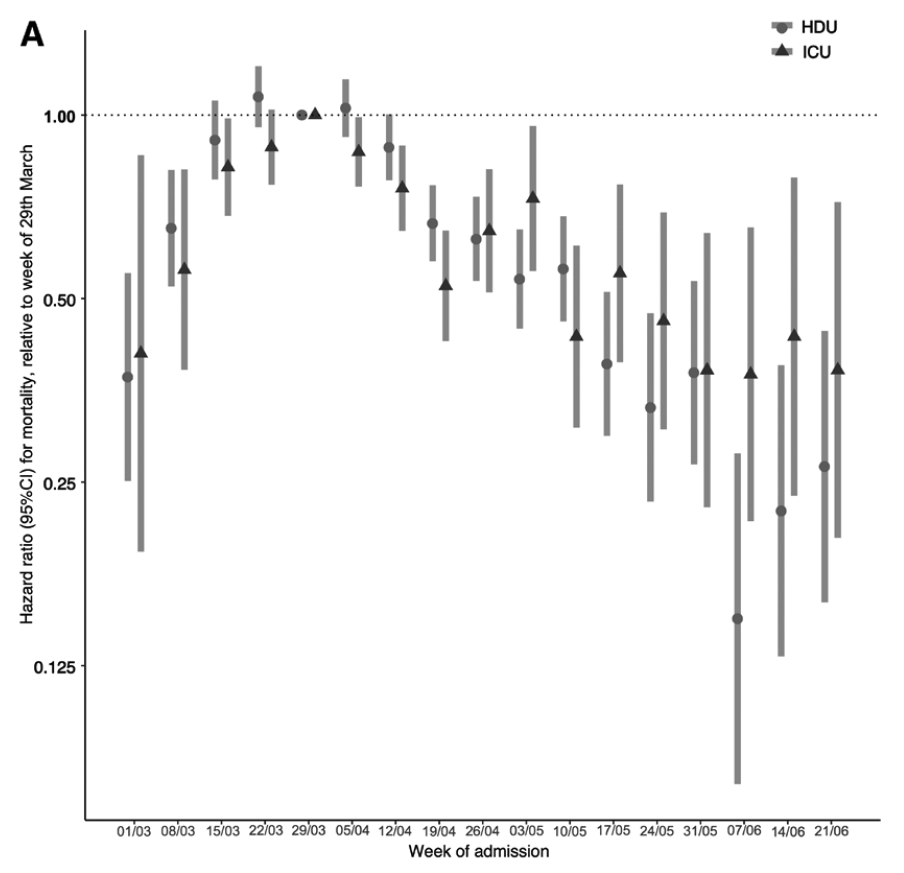
Dennis et al.
In addition to studies of hospitalized patients, a recent modeling study by Yang et al. found a similar pattern when looking at estimated infection fatality rates in New York City. Among people 65 to 74 years of age, the infection fatality rate declined from a high of 7% in early April to 4% in late May; among those 75 years and older, infection fatality rates declined from 19% to 10%. Infection fatality rates showed no change among people under 45. An analysis of publicly available case and death data from Germany also found decreasing case fatality rates over time overall, and specifically for those over 80 years old (a decline from 29% to 11%) and those 60 to 79 years old (a decline from 9% to 2%). There was no change in the case fatality rate among those 35 to 59 years old.
The decline in mortality among older people with COVID-19 is important given the relatively high mortality rates among this age group. There are several possible reasons for the observed declines. Although two of the studies controlled for age and comorbidities and the other two examined older age groups, it’s still possible that there are differences in the populations that were not detected in the data. Frailty among older people, which increases the difficulty of returning to normal after a stress such as illness, can operate independently of measured comorbidities and could leave people more vulnerable to severe illness and death due to COVID-19. For instance, an 85-year-old with hypertension who needs full-time care in a nursing home may be much more vulnerable than an 85-year-old with hypertension who remains at home and is fully able to care for themselves.
Another potential reason for the decline in mortality is improvements in hospitals’ ability to care for COVID-19 patients. Treatments that have been shown to be effective in clinical trials are now being used. Dexamethasone reduced mortality by 18% among patients who received oxygen and by 34% among those who were on mechanical ventilation. There is evidence suggesting that patients who have difficulty breathing have improved oxygenation if they are turned to a prone position (face down). Finally, there has been a standardization of care for COVID-19 patients. The Infectious Disease Society of America and other expert medical organizations have issued guidelines for the management of patients with COVID-19, drawing on what is already known about caring for patients with viral pneumonia as well as new evidence about COVID-19 specifically. All of these advances have likely improved outcomes for patients, but it is unclear whether these advances account for the substantial decline in mortality.
Another possible explanation is that hospital care improved simply because hospitals are no longer overwhelmed. In the study from England, mortality actually went up between early March and early April, peaking at the same time as hospital occupancy, before both decreased. Similarly, the estimated infection fatality rate in New York City increased throughout the month of March. At the peak of the New York City epidemic, emergency responders were deciding who was sick enough to go to the hospital because hospitals and emergency rooms were so crowded. Critical care for severely ill patients, including moving patients to a prone position, takes intensive resources to implement successfully. Unfortunately, this means that as COVID-19 cases rise in the United States and Europe, we could see mortality rates increase again as hospitals fill up and providing high-quality care becomes more challenging.
Finally, it’s possible that there is a change in the virus itself or in how people are becoming infected. In a previous science review, we looked at the hypothesis that masks and social distancing are reducing the infectious dose of SARS-COV-2, the virus that causes COVID-19, therefore decreasing the severity of disease. While plausible, this is still a hypothesis and remains controversial. Another hypothesis is that the virus is decreasing in virulence over time as it adapts to its host. This is less likely; scientists tracking mutations to COVID-19 have found some indication that it might have become more contagious, but there is no evidence of decreasing severity to date.
In summary, the changing age structure and prevalence of underlying illnesses have contributed to falling mortality rates from COVID-19 over time, but it is not the only factor.
National COVID-19 websites
It may be months or years before we fully understand what led to the relative success of some countries, such as New Zealand and South Korea, in controlling the spread of COVID-19. Although questions remain about optimal strategies to communicate risk, keep the public informed, and engage communities in the response, a critical component of government response to any public health crisis is communication with the public. In order to capture government communication practices from around the world, we reviewed national and public health agency websites from a sample of countries. We looked at different practices related to risk communication and public health messaging, using language translation software to interpret the information on some sites. We identified seven topic areas to assess that encompass not only disease-specific information but also information relevant to the overall health and well-being of individuals and communities. These seven topics are:
- risk level
- situation updates
- basic information about SARS-CoV-2, the virus that causes COVID-19
- information about what people should do to reduce risk
- details about the response
- options for financial relief
- where to find more information
South Korea identified its first case of COVID-19 on Jan. 20, 2020, earlier than any of the other countries included in this report. On the president’s website, there is a prominent link to the South Korean Ministry of Health and Welfare’s site for COVID-19. This site provides a cumulative and one-day snapshot of basic COVID-19 epidemiology in the country, as well as links to an official response board, public advice and basic information about COVID-19. Users can access briefings made by public health and government officials on COVID-19, including links to videos on YouTube about international recognition for South Korea’s successes using the 3 T’s: Test, Trace and Treat. The South Korean national site does not provide a risk level framework. However, it does provide links to other government agencies involved in the response, including the Korean Centers for Disease Control.
New Zealand’s national COVID-19 site, titled “Unite Against COVID-19,” prioritizes risk communication and informs the public about actions each person can take to reduce the spread. On the landing site, there are messages about the current level of risk, as well as information about wearing masks and staying home when ill. From the main landing site, there are links to the country’s larger alert level system and regional advice, and the country’s latest COVID-19 updates. There are also links to information about travel; health and well-being; COVID-19 in general; financial resources for businesses and individuals; and managing various aspects of everyday life during the pandemic. The information on the site is available in multiple languages. Some basic case and death information is available on the site’s update section. More granular epidemiologic data is available on the New Zealand Ministry of Health site which can be accessed through a link on the main site.
Mexico’s national government website provides a prominent link to the country’s COVID-19 website. Here, there are 25 additional “button” links to specific topic areas such as caring for the elderly during the pandemic, contact information for COVID-19 resources in individual states and localities, myths about COVID-19, and frequently asked questions. There is also a formal risk alert system called the “traffic light” which informs people about the current national level of risk as well as some brief information about what actions are necessary at each level. There is also an embedded video from the public health ministry with a color coded map that shows the degree of disease activity by state/locality. As in some other countries, there are links to daily news conferences from country leadership on the state of the pandemic.
Germany’s COVID-19 website displays information about the pandemic and response in a variety of formats. From an “overview” page, users can access a menu that links to basic information about the disease and its spread, frequently asked questions, and updates on financial relief. They can access a variety of educational articles and videos about various aspects of the pandemic as they relate to higher education, freedom of speech, and vaccines, among other topic areas. There are also links to dispelling misinformation about COVID-19, materials in different languages, and infographics that outline the current level of restrictions in the country. An embedded dashboard from the Robert Koch Institute, Germany’s federal public health agency, displays the latest epidemiology by region.
On the landing site of the Uganda COVID-19 “response info hub” there is a snapshot of epidemic metrics in Uganda. There are links to two country dashboards: one with more detailed data on the epidemic and another that presents a countrywide vulnerability index, examining trends in poverty, hospital capacity, demographics and other factors by region. There are drop-down menus to access further information on the epidemic timeline and response in Uganda. There is a document repository that includes links to nearly 200 documents from the Africa Centers for Disease Control, the World Health Organization (WHO), the Uganda Ministry of Health, other government and nongovernmental organizations, and experts on a variety of topics. The repository can be searched several ways including by author, topic or sector. There are situation reports, press releases, response plans, guidelines for different sectors and information on public health and social measures to keep communities safe. There is a separate section of resources on risk communication and social mobilization, which is one of eight response pillars presented on the website. There is no risk level system.
The most obvious link on the Government of Canada COVID-19 website, via a large button at the top of the page, is to a COVID-19 Alert application that uses phone location data to inform users whether they have been near someone who has tested positive in the past 14 days. This application has been downloaded more than 5 million times. The rest of the landing page is formatted as a series of links within several topic areas including a situation report, resources for financial support, health information on topics including but not limited to COVID-19, information on public health and social measures, and guidelines specific to different sectors and populations. The entire website is available in both French and English, and some resources are available in additional languages. Within each link there are multiple links to a number of subtopics; much of the linked information is covered via text that is comprehensive while also clearly and succinctly presented.
| South Korea | New Zealand | Mexico | Germany | Uganda | Canada | |
|---|---|---|---|---|---|---|
| Risk level | ||||||
| Situation updates | ||||||
| Information about virus | ||||||
| What people should do | ||||||
| Response details | ||||||
| Financial relief | ||||||
| More information |
The country COVID-19 websites we assessed illustrate a variety of approaches to communicating information on the pandemic. As the pandemic has had dramatic impacts on health and well-being beyond just those associated with infection risk, we looked for information on the pandemic and several pillars of the response, including risk communication. All websites we assessed provide comprehensive information including a situation report and guidance on public health and social measures. Although all country websites include communication about disease risk, we found the most variability in whether or not a country provides a risk alert level system.
We did not assess websites for usability, and specifically on how easy or difficult it was to access certain types of information. It is important for countries to provide their citizens with a centralized resource that contains country-specific and evidence-based information on multiple aspects of the pandemic and the response from a whole-of-society approach. This may be one of the best ways to empower people to make informed safety decisions, understand current issues and how those issues are being addressed, and to feel that they are part of a cohesive, supportive response to the most challenging public health crisis faced by humanity in over 100 years.
Weekly Research Highlights
Birth and Infant Outcomes Following Laboratory-Confirmed SARS-CoV-2 Infection in Pregnancy — SET-NET, 16 Jurisdictions, March 29–October 14, 2020
(MMWR, Nov. 6)
- Researchers at the U.S. Centers for Disease Control gathered surveillance information on pregnant women who tested positive for SARS-CoV-2 and analyzed information on birth outcomes when these were available.
- Information was available on 5,252 women who tested positive for SARS-CoV-2 during pregnancy. For 3,912 of these, information was available about gestational age at the time of live birth. Among the live births with known gestational age, 13% were preterm (less than 37 weeks) compared to a national estimate of 10% from 2019. A small proportion of babies born to mothers with known COVID-19 also tested positive for infection, however none of these occurred in women who had infection more than 14 days prior to delivery.
- Although there are limitations to conclusions that can be drawn from retrospective research from surveillance data which may sometimes be incomplete and not controlled for potentially confounding risk factors, pregnant women should be counseled about the potential risks of COVID-19 during pregnancy including the possibility of preterm birth. Pregnant women and those in their household should take measures to reduce risk of COVID-19 including the 3 W’s.
COVID-19 Outbreak at an Overnight Summer School Retreat ― Wisconsin, July–August 2020
(MMWR, Oct. 30)
- An outbreak investigation at an overnight summer retreat for high school-aged boys held in Wisconsin documented rapid spread of COVID-19 among attendees and staff. Despite testing and pre-arrival quarantine requirements for attendees, more than three quarters of attendees eventually developed confirmed or probable COVID-19.
- Among 24 attendees who had a positive serologic test for SARS-CoV-2 antibodies at the time of arrival, no cases were identified. Given the high attack rate among attendees overall and zero rate of infection in those with documented antibodies, this may be preliminary evidence that antibodies may provide some protective effect for an unknown period of time, although the data from this investigation are not definitive. However, the likelihood that none of 24 people with prior positive antibody tests would have a positive RT-PCR test while 116/128 others who were tested received a positive test would occur by chance is essentially nil. Along with other outbreak studies, such as one from a fishing boat, this provides highly suggestive evidence that at least some people with prior infection are protected at least for some time from repeat infection.
- Infectious diseases including COVID-19 can spread rapidly in congregate settings. Strict adherence to mitigation measures are necessary to reduce the risk of outbreaks in these settings. Once cases are identified, rapid testing, isolation and quarantine are necessary to minimize spread; prompt engagement with public health officials may be necessary in these settings.
SARS-CoV-2 Seroprevalence and Transmission Risk Factors Among High-Risk Close Contacts: a Retrospective Cohort Study
(Lancet Infectious Diseases, Nov. 2)
- Close contacts were defined as people who had contact with someone with COVID-19 within 6 feet for at least 30 minutes (in Singapore, guidelines stipulated that all close contacts were monitored under quarantine for 14 days; those who developed symptoms underwent PCR testing for SARS-CoV-2). Between January and April, PCR testing detected 188 COVID-19 cases among 7,770 close contacts of 1,114 index COVID-19 cases, yielding attack rates of: 5.9% (95% CI 4.9–7.1) for 1,779 household contacts; 1.3% (0.9–1.9) for 2,231 work contacts; and 1.3% (1.0–1.7) for 3,508 social contacts.
- Serologic testing data showed that the symptom-based PCR-testing strategy missed ~60% of COVID-19 diagnoses.
- Analysis of data from a 70-point risk factor questionnaire showed that risk factors for infection among household contacts included sharing a bedroom with an index case (OR 5.38 [95% CI 1.82–15.84]) and being spoken to by an index case for 30 minutes or longer (7.86 [3.86–16.02]). Among non-household contacts, risk factors for infection included exposure to more than one case (3.92 [2.07–7.40]), being spoken to by an index case for 30 minutes or longer (2.67 [1.21–5.88]), and sharing a vehicle with an index case (3.07 [1.55–6.08]).
- Not all contacts underwent serologic testing so there may have been a testing bias. Potential effects of mask use were difficult to assess: mask use among index cases was high (>80%), while mask use by close contacts “during all contact episodes” was low (<10%). A difference in mask use could not be detected between case-contact pairs where there was transmission in comparison with pairs without transmission.
Suggested citation: Cash-Goldwasser S, Jones SA, Bochner A, Cobb L and Frieden TR. In-Depth COVID-19 Science Review October 31 – November 6, 2020. Resolve to Save Lives. 2020 November 12. Available from https://preventepidemics.org/covid19/science/review/