Data Insight:
Estimated impact of COVID-19 on life expectancy in New York City
To date, New York City and the surrounding metropolitan area have seen the largest COVID-19 outbreak in the world. A recent publication reported that of the 32,107 deaths in New York City between March 11 and May 2, 24,172 were “excess deaths,” meaning deaths caused either directly or indirectly by the COVID-19 epidemic. The 1918 Spanish flu caused life expectancy to drop in the United States by 12 years between 1917 and 1918 (Figure). We wanted to understand what impact these excess deaths to date might have on one of the key tools the city uses to measure the health of its citizens: life expectancy. Using data reported by the New York City Department of Health through May 14, 2020, we estimated that the excess deaths to date in this first wave of the pandemic of COVID-19 likely caused a drop in life expectancy of five years. This should be seen as a preliminary estimate of the potential scale of the impact as there will be more deaths due to COVID-19, our methods were simple and the limited amount of publicly available data required us to make many assumptions. A more methodologically rigorous and complete analysis is needed.

In-depth topics
COVID-19 and surface contamination
Similar to other respiratory viruses, SARS-CoV-2 is transmitted in respiratory droplets expelled when an infected person sneezes, coughs, speaks or breathes. When these droplets fall onto a surface, detectable virus can persist for hours or even days. It is almost certain that some cases occur when others come into contact with these infected surfaces. In a laboratory experiment, researchers compared how long a known quantity of SARS-CoV-2 lasted after it was applied to four different surfaces. Some living virus was detectable after 72 hours on plastic, stainless steel, copper and cardboard, but the amount that remained diminished over time—especially on copper and cardboard. In a comparable study that was carried out to seven days, virus persisted on surfaces and on examination gloves and surgical masks; but it was rapidly inactivated (starting in as little as one hour) on paper or clothing at room temperature. Other human coronaviruses can remain infectious on environmental surfaces for as long as nine days, but they are easily inactivated with alcohol, bleach or hydrogen peroxide. How long a virus remains infectious in the environment is also shortened when the ambient temperature is higher than 30°C.
It is harder to know what these experimental studies tell us about natural transmission during the ongoing pandemic. Viral material and living virus can be found in areas where COVID-19 patients have been cared for, especially on high-touch surfaces such as doorknobs and handrails, computer keyboards and mouse devices, toilets, floors and trash cans—even personal protective equipment and hand sanitizing stations. In most investigations of COVID-19 clusters, including superspreader events, nearly all the secondary cases have had extensive interpersonal contact with another case patient, and could easily have become infected either by inhaling droplets or touching contaminated surfaces. A small number of transmission chains seem to indicate that people became infected after touching items or sitting in a seat after an infectious person, without any documented interpersonal contact. Although the proportion of SARS-CoV-2 transmission that occurs through surface contact may be substantially lower than the proportion that occurs through respiratory contact, the risk is unlikely to be trivial. Precautions that call for frequent handwashing and decontamination of surfaces in health care settings, households and public spaces are, therefore, strongly recommended to reduce transmission of COVID-19.
The changing landscape of COVID-19 diagnostics
Different test modalities may detect distinct targets (i.e. the pathogen itself versus the immune response to the pathogen). Tests may require specimens that must be obtained invasively (i.e. blood) or necessitate sophisticated technology for processing, which can affect where a test can be performed, how long it takes to produce results, and how much it costs. Critical parameters of any test are its discriminative properties, including sensitivity (the probability of getting a positive result in someone who has the disease) and specificity (the probability of getting a negative result in someone who doesn’t have the disease). These influence the ability of a test to distinguish those who have the disease from those who don’t; a test with low sensitivity may not detect the disease and may therefore produce a false negative result. The discriminative properties of a test may be affected by many factors, including the type of sample (i.e. sputum versus saliva) and the quality of sample collection. Recent changes in the landscape of COVID-19 diagnostics in the United States can be considered through three lenses: 1) test type, 2) sample collection site, and 3) sample type.
- Test type: On May 8, the US Food and Drug Administration (FDA) issued its first Emergency Use Authorization (EAU) for a COVID-19 antigen test. Antigen tests are a different test modality than previously authorized molecular tests, which detect SARS-CoV-2 genetic material, and antibody tests, which detect an immune response to SARS-CoV-2. Antigens are substances to which the immune system may react; antigen tests for SARS-COV-2 are designed to detect viral proteins. Antigen tests, like molecular tests, are best for detecting acute infections because they detect parts of the pathogen. Antigen tests can be simpler and cheaper to make and faster to run; the FDA-authorized SARS-CoV-2 antigen test can be processed in 15 minutes. However, many antigen tests have low sensitivity–that is, they report negative results for some people who have the infection. Lessons can be learned from rapid influenza diagnostic tests (RIDTs) which can detect influenza antigens in 10-15 minutes with high specificity but only moderate sensitivity. Thus, expert guidance on the use of RIDTs emphasizes not basing treatment decisions solely on negative RIDT results. New guidelines raising the bar for RIDT diagnostic sensitivity in order to gain FDA approval were issued in 2017, given concerns about the risks false-negative RIDT results may pose to patients and public health. Indeed, for the newly authorized SARS-CoV-2 antigen test, the FDA states that ‘negative results should be treated as presumptive and confirmed with a molecular assay.’ The World Health Organization (WHO) currently recommends against the use of antigen tests to diagnose COVID-19. Although antigen tests are attractive to COVID-19 control efforts because they can be easily made, quickly run and rapidly scaled, it is critical to determine their diagnostic accuracy. The major use of antigen tests may be to “rule in” infection; a negative test may not rule out infection. This can be useful in many settings.
- Sample collection site: The US Centers for Disease Control and Prevention (CDC) has recently removed a stated preference for nasopharyngeal swabs to diagnose COVID-19 and endorses the use of two sample collection sites: the nasopharynx (NP), or the back of the nasal cavity over the soft palate, and the oropharynx (OP), or the throat. This is in contrast to FDA recommendations that OP samples be used only if NP sampling cannot be done. In further contrast to both organizations, the WHO recommends that OP samples may be used in combination with NP samples. There are not robust data to support OP sampling to diagnose COVID-19. Two non-peer reviewed studies have compared viral detection rates between NP and OP samples; these studies were not designed to draw definitive conclusions about the discriminatory capacity of tests using samples from different sites. One study showed no discernible differences in viral load or detection rate when comparing NP and OP results and the other study showed that tests using OP swabs detected SARS-CoV-2 less frequently than tests using NP swabs, especially later in the course of illness. The performance of tests using OP versus NP samples has been assessed for other respiratory viruses: a large study of over 2,000 paired OP/NP samples found that neither sample type performed uniformly better for all viruses, and another study showed that OP sampling was less sensitive than NP sampling to detect influenza viruses, coronaviruses, and rhinoviruses. Differences in viral detection rates may depend on viral affinity for different parts of the respiratory tract. If sample collection is difficult for a healthcare worker or uncomfortable for a patient, lower-quality samples may be obtained. Although further study on sample site preference to diagnose COVID-19 is needed, this pandemic may warrant consideration of issues that would not normally influence testing recommendations. For example, specific equipment that may be in short supply is required to collect and process different sample types, and it may be reasonable to perform relatively less-than-optimal testing if the alternative is performing no testing at all. Differences in expert guidance may reflect both scientific and practical considerations.
- Sample type: The FDA has recently granted an Emergency Use Authorization (EUA) for a SARS-CoV-2 saliva test. SARS-CoV-2 may be present in a range of body fluids but testing for COVID-19, as for other respiratory disease, has focused primarily on respiratory tract samples. Samples that can be obtained with minimal burden to the patient are potentially valuable for several reasons, including to reduce the risk to healthcare workers from invasive collection methods and to allow patients to collect their own samples. Indeed, although the newly authorized COVID-19 salivary test is run in a lab, the sample may be self-collected at home. There are scant data to support the use of salivary testing to diagnose COVID-19. In one study, salivary samples from 25 COVID-19 patients all tested positive for SARS-CoV-2. A non-peer reviewed study that included molecular testing for SARS-CoV-2 on 38 pairs of salivary/NP samples from COVID-19 inpatients found virus in salivary but not in NP samples from eight sample pairs (21%), although virus was detected in NP but not in salivary samples in three matched samples (8%). Similar to the studies on NP versus OP sampling, this study was not designed to draw definitive conclusions about salivary test discriminatory capacity, and results may not be generalizable to other patient populations. At this time, neither CDC nor WHO endorse salivary testing for COVID-19 diagnosis.
COVID-19 immunity certificates
Several governments have discussed issuing ‘immunity passports,’ or government sanctioned certifications attesting that holders have immunity to SARS-CoV-2, the virus that causes COVID-19. One intended use of immunity passports would be to exempt holders from restrictions that aim to mitigate epidemic spread. However, there is currently insufficient scientific evidence to support claims of protection from COVID-19 based on antibody testing. Even if our understanding of immunity to SARS-CoV-2 progresses to the point that antibody testing could reliably predict protection from COVID-19, any immunity passport program would still need to overcome various legal and ethical issues. Although we reference government-sponsored passport programs to frame this discussion, the scientific, ethical and legal questions raised here are relevant to other potential applications of antibody test results, such as work restrictions on hospital employees or the grouping of nursing facility residents by antibody status.
The human immune system includes a highly complex array of organs, cells and proteins. Some of these proteins are antibodies, which are produced by immune cells to fight infections and prevent re-infection. It is plausible that antibodies produced in response to COVID-19 can aid recovery from COVID-19 and then be reactivated, potentially preventing re-infection or reducing the severity of a second infection.
There are several critical scientific unknowns that should limit the implementation of any immunity passport program. First, how much the presence of antibodies to SARS-CoV-2 predicts protection against COVID-19 is unknown. Some recovered COVID-19 patients have tested negative for antibodies, although the performance characteristics of the tests used are not known. Different people may produce varying amounts of several separate antibody types in response to the same pathogen, and correlations between SARS-CoV-2 immunity and the type and degree of the antibody response are not well described. Second, there is uncertainty about how long immunity to SARS-CoV-2 lasts, and time will be required to determine the duration of immunologic protection. Although data on the human immune response to other respiratory viruses are available, extrapolating from other pathogens to SARS-CoV-2 is problematic. Third, the degree of desired protection, and the antibody correlates of that degree of protection, would need to be determined. Would antibodies need to protect completely from re-infection or just prevent severe disease? We know from other human coronaviruses that antibodies may not be fully protective against re-infection but may reduce the severity of reinfection. Such re-infected individuals, with mild or asymptomatic COVID-19, may still spread the virus. Lastly, there are questions around the accuracy of antibody tests. Inaccurate results leading to exemption from public health and safety measures could seed and drive new outbreaks.
It could take years to attain a complete understanding of human immunity to SARS-CoV-2. Even if our scientific understanding of immunity to SARS-CoV-2 advances significantly, additional study of the behavioral, economic, legal and ethical implications of introducing an immunity-based policy would be needed. There could be many issues including perverse incentives, muddled risk communication messages, violations of patient privacy, diversion of resources, fraudulent certificates, and creation and perpetuation of inequalities, among others.
Weekly Research Highlights
Preliminary Estimate of Excess Mortality During the COVID-19 Outbreak – New York City, March 11 – May 2, 2020
(MMWR, Early Release 11 May 2020)
- Using New York City’s electronic vital statistics reporting system, the authors compared the expected seasonal baseline mortality to the actual mortality measured from March 11 to May 2, 2020.
- Of the 32,107 total deaths reported during this time period, 24,172 were found to be in excess of the expected mortality if the pandemic had not occurred. The 13,831 confirmed and 5,048 probable COVID-19 deaths leave 5,293 excess deaths. These may be due to false-negative SARS-CoV-2 tests, or lack of availability to care for routine conditions.
- This report is limited in that it cannot establish a causal relationship between the pandemic and unaccounted excess deaths but establishes a temporal association.
Identification and Monitoring of International Travelers During the Initial Phase of an Outbreak of COVID-19 – California, February 3 – March 17, 2020
(MMWR Early Release 11 May 2020)
- The California Department of Public Health (CPDH) received information for 11,574 international travelers to 51 of 61 local health jurisdictions. These records were reviewed by CPDH staff for completeness and errors prior to being passed on to local health departments for follow up, interviews, quarantine, and self-monitoring instructions.
- CPDH staff contributed 1,694 hours of personnel time with a significant proportion outside regular work hours in order to perform this review and transmission of information. The most common errors in the information collected included lacking a correct US-based telephone number, which occurred in 75% of the 1,523 records with errors, and duplicate records.
- Limitations included the inability of screening to capture asymptomatic cases. Documented community transmission and need for mitigation strategies reduced the potential impact of screening travelers and efforts aimed at containment.
An Outbreak of severe Kawasaki-like disease at the Italian epicentre of the SARS-CoV-2 epidemic: An observational cohort study
(Lancet 13 May 2020)
- By retrospectively examining the records of patients admitted to a pediatric hospital from January 1, 2015 to April 20, 2020, the researchers were able to compare the incidence of Kawasaki Disease before and after the start of the SARS-CoV-2 epidemic.
- In the five years prior to Italy’s SARS-CoV-2 epidemic, 19 cases of Kawasaki Disease were identified, compared to 10 cases after the start, for an increase in incidence rate from 0.3 cases per month before the pandemic to 10 cases per month after the start of the COVID-19 pandemic. The average age of the patients was higher during than before the pandemic (7.5 years vs 3 years) as was the proportion with shock as part of the clinical picture (50% vs 0%). Among those diagnosed after the start of the epidemic, 8 of 10 had antibodies to Sars-CoV-2. All of the patients in this series recovered.
- The authors acknowledge that the recent patients represent a small case series, but emphasize the strong link to SARS-CoV-2 and more severe Kawasaki-like disease.
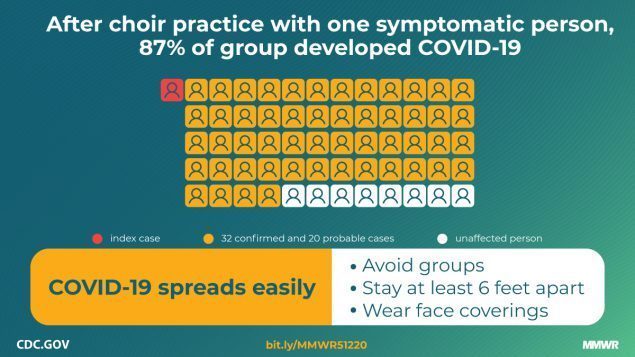
High SARS-CoV-2 Attack Rate Following Exposure at a Choir Practice – Skagit County, Washington, March 2020
(MMWR Early Release, 12 May 2020)
- The authors describe a superspreading event at two choir practices attended by 122 members. A likely index case developed symptoms on March 7. All choir members were interviewed to establish potential exposure to the index case from choir practices on March 3 and March 10 and assessed for symptoms of COVID-19.
- A cluster of 52 secondary cases was identified, yielding an overall attack rate of 53% among confirmed cases, and 87% when including probable cases.
- Inability to obtain actual seating arrangements limits further analysis into proximity of secondary cases to the index case. A proportion of cases were probable and did not undergo confirmatory testing.
Suggested citation: Cash-Goldwasser S, Kardooni S, Cobb L, Bochner A, Bradford E and Shahpar C. In-Depth COVID-19 Science Review May 10 – 17, 2020. Resolve to Save Lives. 2020 May 19. Available from https://preventepidemics.org/covid19/science/review/