A Hidden Toll: The Mental Health Impacts of COVID-19 on the Public Health Workforce
What is the role of public health workers in the COVID-19 response?
During the COVID-19 pandemic, public health professionals around the world have investigated the epidemiology of SARS-CoV-2, a novel pathogen, and worked to control its spread. In the U.S., where the government public health system consists of local health departments, state health departments, 12 Tribal Epidemiology Centers and the federal Centers for Disease Control & Prevention (CDC), there are approximately 97,000 state and 147,000 local public health workers employed by the government. Responsibilities taken on by public health professionals have included the following:
- Collecting, reporting and interpreting epidemiologic data;
- Developing and issuing public health recommendations;
- Providing technical assistance with infection prevention and control, including in high-risk settings such as long-term care facilities;
- Investigating outbreaks and superspreading events;
- Conducting case investigations and contact tracing;
- Planning and implementing COVID-19 testing and vaccination programs;
- Screening travelers for SARS-CoV-2 infection.
Outside of the U.S., public health workers have taken on many of these same responsibilities. In some countries, public health workers may also perform clinical roles. For example, in many low- and middle-income countries, community health workers deliver both primary health care and public health services, especially in rural and underserved settings. Community health workers educate community members about healthy behaviors, such as COVID-19 prevention measures, and may conduct contact tracing, transport, screening and follow-up of patients with COVID-19. They often come from the vulnerable communities they serve, which may make them more susceptible to COVID-19 as well as to mental health issues due to the impact COVID-19 may have on their own communities.
How has the COVID-19 pandemic affected mental health of public health workers?
Responding to the COVID-19 pandemic, the largest public health crisis many public health professionals have ever faced, has resulted in substantial mental stress for these workers. In addition to undertaking new, expanded professional responsibilities, they have faced mixed and sometimes hostile reactions to their work from political leaders and the public. Like workers in other fields, they have also experienced fear of contracting COVID-19 on the job and increased responsibilities at home, such as for childcare.
At least three surveys have investigated the mental health effects of the COVID-19 pandemic on the public health workforce. One was conducted in China and two in the United States. All were cross-sectional, anonymous, online surveys focused primarily on public health workers employed by government agencies.
The first survey was conducted in February and March 2020 in five Chinese provinces. Chinese public health workers included in the study were responsible for activities such as COVID-19 testing, epidemiological investigation, contact tracing, disinfection of public spaces, community prevention and control activities, data collection and reporting and delivery of health education. Four papers have reported on different aspects of this survey and its findings. Among 9,475 respondents, 49% reported symptoms of psychological distress; 27% reported depression and 21% anxiety. As potentially contributing factors, 40% reported lack of cooperation from the public and 14% reported verbal abuse or intimidation. Among a subset of 3,417 respondents who self-reported mental health concerns, only 13% reported seeking professional mental health care. Those who did not seek care reported that mental health was not a priority during the pandemic, that they lacked time and access to services, or that they did not believe treatment would be useful. Most respondents perceived a low level of support from the workplace and society.
The studies’ authors suggested that strain on Chinese public health workers was exacerbated by workforce shortages, limited societal appreciation of the importance of public health work and the likelihood that certain responsibilities (e.g., enforcing quarantine) would elicit negative emotions. To improve mental health during emergency responses, the authors proposed: increased communication with communities to increase appreciation for and trust in public health workers, allocating resources to ensure a sufficient workforce and continuing education, and skill-building opportunities for public health workers to cultivate resilience. Authors also suggested that pandemic preparedness plans include mental and physical support for public health workers.
The second survey was conducted in August and September 2020 among 225 public health workers from 31 U.S. states and Washington D.C., 79% of whom worked in government agencies (the remainder in academic or other settings). Forty-one percent of respondents reported symptoms of anxiety, 29% reported symptoms of depressive disorder, and 66% reported burnout. One in five respondents reported reductions in activity outside work due to poor mental or physical health in the past month. Older age and more years of experience were associated with higher levels of burnout. In January 2020, five percent of respondents planned to leave or retire in one to two years. By September—half a year into the pandemic—this share had more than doubled (12%). The authors suggested that increased funding and workforce development were essential to improve mental health among public health workers.
The third and most recent survey was conducted in March and April 2021 and included 26,174 respondents employed by state, tribal, local or territorial U.S. health departments in 2020. Approximately half (53%) of participants reported symptoms of at least one mental health condition in the past two weeks: 32% reported symptoms of depression, 30% anxiety, 37% post-traumatic stress disorder (PTSD) and 8% suicidal ideation. The authors noted that the prevalence of symptoms reported by public health workers was higher than reported in a similar survey by the general public, and similar to rates reported by health care workers. The severity of mental health symptoms among respondents increased with increasing hours worked per week and percentage of work time dedicated to COVID-19 response. Workers unable to take time off were twice as likely to report symptoms. Most (72%) respondents felt overwhelmed by workload and 23% felt bullied, threatened or harassed because of their work, including 12% who had received job-related threats. One in five survey respondents reported needing, but not receiving, mental health counseling/services in the past four weeks, and only 12% had used employee assistance programs, although two thirds had access to such programs.
These studies are subject to at least four important limitations. First, all three surveys were cross-sectional and did not explore respondents’ mental health history. As a result, it is not clear whether mental health concerns reported by respondents existed before the pandemic and to what extent symptoms were due to or may have changed during the pandemic response. Second, all studies relied on a convenience sample of respondents and were not able to assess response rate. It is not possible to predict whether and to what extent self-selection to participate in the studies may impact findings—persons experiencing mental health concerns might be more or less likely to respond to the survey. Third, findings from studies done in China and the U.S. may not be fully applicable to other countries where public health workers may have different training and roles. Fourth, these studies used different instruments to assess self-reported mental health symptoms; results may not be comparable across studies or with diagnoses made by qualified professionals. Further, definitions of adverse mental health impacts may differ across cultural contexts, underscoring the importance of conducting research using tools validated within the cultural context of the study.
Nonetheless, these three surveys suggest a high prevalence of mental health symptoms among public health workers participating in COVID-19 response. In light of these findings, a critical question is: “What can be done to address mental health impacts of the COVID-19 pandemic and prevent future harm?” In order to develop effective interventions, it is necessary to understand the factors that may contribute to mental health impacts in the public health workforce.
What do we know about risk factors for job-related mental health issues among public health workers?
Threats and/or harassment of public health workers during the pandemic is a major contributor to poor mental health outcomes. As summarized in this commentary, some public health officials have faced protesters at work and at their homes and harassment on social media forums, such as doxing (publishing private information to facilitate harassment). In some cases, these threats necessitated assignment of security details.
In the United States, between the start of the pandemic and August 2020, 18 of 59 state or territorial health officials had left office, along with at least 37 county/city health officials. Approximately one third of resignations were linked to conflicts with elected officials or threats from the public. Between March 2020 to January 2021, media reported on at least 190 departures of leaders from health departments across the country. Departures at the leadership level may be particularly disruptive to organization operations and strategy, further increasing strain on the remaining staff. The turnover among non-leadership public health workers remains largely unquantified.
In the United States, a shortage of public health resources, including human resources, may also have contributed to poor mental health outcomes among public health workers. Since 2008, local health departments in the U.S. have lost 31,000 jobs, while state health departments have lost approximately 10% of their workforce and 10% of funding since 2012. Another study estimated even larger losses: as many as 56,000 local health department jobs lost since 2008. As of 2020, the Prevention and Public Health Fund – established to improve and sustain national public health systems in 2010 as part of the Affordable Care Act – had received only half as much money as originally planned.
Unfortunately, the literature does not provide robust information about risk factors that might lead to worse mental health outcomes among public health workers. For example, studies did not explore whether worse mental health was associated with specific job functions, professional training or level of responsibility within the organization. In the absence of such data, we may look to existing literature on risk factors for mental health problems among health care workers who have also experienced immense challenges during the pandemic.
Health care workers
Health care workers also have suffered adverse mental health impacts due to the COVID-19 pandemic. This may not be surprising: compared with other occupations, health care workers are at a relatively high risk of mental health symptoms and conditions even under usual work conditions; this risk is heightened during epidemics and pandemics. The extent of the issue during the COVID-19 pandemic has been recognized by CDC and the World Health Organization.
Multiple systematic reviews encompassing hundreds of studies have found that health care workers were at an increased risk of developing mental health conditions such as anxiety, depression and symptoms of PTSD during the COVID-19 pandemic. For example, one systematic review included 65 studies written in English or Chinese that were conducted between December 2019 and August 2020. Among 97,333 health care workers across 21 countries, depression, anxiety and PTSD were each detected in more than 20% of participants.
There is comparatively more literature on the factors that may contribute to poor mental health outcomes among health care workers during the COVID-19 pandemic than there is on factors that may impact public health workers. A systematic review of studies on mental health impacts of the pandemic on health care workers which included 22 studies reporting variables associated with mental health symptoms found that the most commonly reported risk factors were female sex, contact with COVID-19 patients and concern about being infected or family members being infected. A study that enrolled 20,947 US health care workers between May and October 2020 found that 38% reported anxiety or depression and 49% reported burnout, found that stress was highest among nursing assistants, medical assistants and social workers, and was higher in inpatient than outpatient workers, in women than in men, and in Black and Latinx workers than in White workers. A cross-sectional study from Turkey on anxiety levels among 402 emergency medical services professionals (paramedics, emergency medical technicians, nurses, physicians and drivers) found that female and younger participants, as well as those who thought they had inadequate personal protective equipment or did not feel safe treating people with suspected or diagnosed COVID-19, had higher anxiety levels. Among nearly 4,000 police, fire and ambulance services surveyed in the United Kingdom, 69% reported declining mental health over the past year.
Studies from low and middle income countries, for example from Ghana, Kenya, Brazil, Mexico and India, also describe a high prevalence of mental health symptoms among health care workers during the pandemic. In low and middle income countries, health care systems have been overwhelmed, shortages of basic equipment have led to difficult triage decisions and poor health care worker safety, and some health care workers have abandoned their posts due to fear of COVID-19 or targeting and harassment by the public, while many others have died of COVID-19. Some experts fear a wave of health care workers leaving their jobs after the pandemic, further exacerbating the global health care worker shortage.
Some of the risk factors elucidated by studies of mental health impacts among health care workers, such as sex, age and work experience, may be risk factors for poor mental health outcomes among workers across a range of professions. Some, such as fear of contracting COVID-19 at work and pressures associated with responding to an unknown health threat, may be risk factors common to health care and public health workers. Other factors may be specific to the health care workforce given unique responsibilities such as caring for severely ill COVID-19 patients who are isolated from loved ones, providing treatment for COVID-19 patients when options are limited and working during COVID-19 surges when hospitals are over capacity.
What can be done to support improved mental health among public health and health care workers?
Effective strategies to better protect the mental health of workers in public health and health services during this and future pandemics must be identified and implemented. Some interventions may be needed at the societal and policy levels and others within workplaces. There is no evidence from the COVID-19 pandemic on the effectiveness of specific interventions to protect these public health workers’ mental health. However, some organizations have made recommendations tailored to the public health workforce that build on strategies known to reduce workplace stressors and address challenges reported by health workers during the pandemic.
Mental Health America outlined eight steps individual public health workers can take to combat frustration and mental health challenges during the pandemic. To support those working in medical or public health services, the Oregon Health Authority is using the PsySTART system, a pre-existing simple mental health triage and rapid treatment system. At the organizational level, implementing “B-team” style crisis management 一 wherein leadership is divided between the “A-team” managing crisis response operations and a “B-team” responsible for maintaining routine agency activities 一 can reduce strain on public health leaders. The Association of State and Territorial Health Officers (ASTHO) has recommended other ways to foster a healthy organizational culture that increases resilience and thus promotes worker mental health. Examples include using the Joy in Work framework, encouraging self-care practices and providing training for supervisors to recognize and act on symptoms of mental health concerns among employees. ASTHO also recommended that emergency response scenario planning include mechanisms to monitor scheduling and workloads, plans for staff to take leave through job rotations and limits on overtime work.
Given the relative abundance of literature of the mental health impacts of the pandemic on health care workers, and shared challenges faced by health care and public health workers, it is worth investigating whether there is evidence on how well interventions to support the mental health of that workforce during the pandemic work. A systematic review of interventions to support the mental health of frontline health and social care professionals during and after an epidemic or pandemic published in November 2020 identified four studies that were conducted during the COVID-19 pandemic. The interventions assessed in these studies were: health care workers adorning their personal protective equipment with an image of their own face in order to improve patient-provider communication and connection; a digital learning package for health care workers which included guidance on actions teams could take to protect mental health, on improving communication and reducing social stigma, and on self-care strategies and managing emotions; a psychological intervention plan that included a medical intervention team and a suite of psychological interventions including group activities to release stress; and a hotline for medical workers through which they could talk to a psychologist. The review included 12 other studies on interventions implemented during other epidemics (Ebola, MERS and SARS). Authors did not have high confidence in the findings about the effectiveness of any of the studied interventions. They did find evidence of at least two barriers to intervention implementation: a lack of full awareness among frontline workers and employing organizations of what was needed to support employee mental health; and a lack of equipment, staff time or skills for an intervention. A November 2020 survey conducted by Kaiser Permanente highlighted that 70% of first responders report seldom or never using mental health services, despite a high prevalence of depression and PTSD in the workforce; authors suggested that strategies to increase first responders’ use of available support services might include reducing stigma by having leaders and peers at work share their own experiences with seeking mental health support. In general, there is a lack of evidence to inform the selection of interventions that are beneficial to the mental health of health care workers.
Strategies known to improve employee wellbeing across a range of occupations and scenarios also may work to promote mental health among the public health workforce. More information about these types of strategies are available from the following organizations:
- CDC recommends workplace mental health best practices;
- WHO offers tips on creating a healthy workplace and models for action;
- The American Psychological Association Center for Workplace Mental Health offers a toolkit for employers, as well as resources for the COVID-19 pandemic;
- Boston College Center for Work and Family offers resources on workplace wellbeing, including related to COVID-19.

Source: CDC
Common themes from these resources are that workplace mental health interventions should be integrated within a broader organizational strategy to foster worker wellbeing and include strategies for prevention, early identification, support and rehabilitation of mental health issues. A key factor in success is involving workers in program development and providing opportunities for employees to participate in decisions about issues that affect job stress.
Conclusion
The pandemic is not over. New surges in COVID-19 cases are compounding mental health strain on responders exhausted by 18 months on the frontlines. Anxiety, depression, trauma and burnout have been commonly reported by public health professionals, health care workers and emergency responders during the COVID-19 pandemic. Addressing these and other mental health concerns among these workers will require focused effort and investment and will be critical to prevent further losses to workforce capacity. The U.S. Department of Health and Human Services will invest $103 million over three years to strengthen resiliency and address burnout among frontline health care workers from paraprofessionals to public safety officers. Research is needed to identify individual-, occupational- and organizational-level risk factors to direct resources to groups at highest risk. Rigorous program evaluations may identify the strategies and interventions that are most effective. While addressing current mental health care needs, continued investigation of preventive measures is also essential to improve worker and organizational preparedness, as well as resilience to face future epidemics and pandemics.
FAQ: Guillain Barre Syndrome and COVID-19 vaccines
What is Guillain Barre Syndrome (GBS)?
- Guillain Barre Syndrome (GBS) is a rare disorder in which the immune system mistakenly attacks the peripheral nervous system (the nerves outside the brain and spinal cord). The CDC estimates that 3,000 to 6,000 people per year in the U.S. develop GBS.
- The resulting nerve damage can result in numbness, muscle weakness and paralysis. Specific symptoms may include vision problems; difficulty speaking or swallowing; unusual sensation in the hands, feet, legs or arms; coordination problems; or difficulty with bladder control. GBS can be a dangerous condition, particularly if the respiratory muscles are affected, and some patients may require intensive care.
- Most people ultimately fully recover though this can take weeks or months.
What causes GBS?
- Cases of GBS have been reported among people infected with SARS-CoV-2, the virus that causes COVID-19. For example, five GBS cases were identified at three Italian medical centers that treated about 1,200 COVID-19 patients during February and March 2020. In these patients, GBS began about 5-10 days after the onset of COVID-19 symptoms, similar to the timing of GBS associated with other viral infections.
- The most common trigger for GBS is a bacterial or viral infection, and many people who develop GBS report a gastrointestinal, sinus or respiratory illness in the weeks or months prior. The incidence of GBS has increased during outbreaks of some diseases, such as the mosquito-borne disease Zika. However, in some cases of GBS, the exact trigger is not established. Male sex is a risk factor for GBS as is older age, and it is more likely to develop in those over 50 years of age.
- Many studies have looked for an association between GBS and vaccines and found none, though a small number of studies have found a very rare association between GBS and seasonal flu vaccines (approximately one case of GBS per one million vaccine recipients when an association has been found, or less than the risk of GBS due to influenza infection).
Do COVID-19 vaccines cause GBS?
- In the U.S., as of June 30, there were about 100 cases of GBS reported among 12.8 million people who have received the J&J vaccine. Most cases occurred within 42 days of vaccine administration. Ninety-five cases required hospitalization and 10 required mechanical ventilation for breathing support.
- This 42-day rate of GBS among J&J recipients exceeded what would be expected in the absence of vaccination among the US population. The FDA has updated the label of the J&J vaccine to warn about a possible increased risk of GBS after vaccination.
- Reports to vaccine safety monitoring systems of GBS among persons who received mRNA COVID-19 vaccines have not exceeded the rate of GBS cases in the general population (Pfizer vaccine: 190 cases, 1.05 cases per million doses administered; Moderna vaccine: 162 cases, 1.21 cases per million doses administered through June 2021).
- Of note, the European Medicines Agency Pharmacovigilance Risk Assessment Committee recommended adding a warning to the label of the AstraZeneca COVID-19 vaccine (by the end of June 2021, 227 cases of GBS had been reported after administration of 51.4 million doses of the AstraZeneca vaccine).
Considering the risk of GBS and the benefit of vaccination, should I get vaccinated against COVID-19?
- Given currently available data, the potential benefits of vaccination (with an mRNA vaccine or with J&J) far outweigh the risk of GBS. mRNA vaccines are not associated with GBS and for J&J, the risk/benefit analysis still favors vaccination.
An analysis conducted by CDC’s Advisory Committee on Immunization Practices (ACIP) used available data to estimate that the number of COVID-19 events prevented by J&J vaccination was substantially higher than the number of expected cases of GBS after J&J vaccination. In the figure below, the right side shows the number of expected cases of GBS and thrombosis with thrombocytopenia syndrome (a very rare event that has also been reported among J&J vaccine recipients) per 1 million vaccine doses, and the left side shows the number of expect COVID-19 cases, hospitalizations and deaths that would be prevented per 1 million vaccine doses.
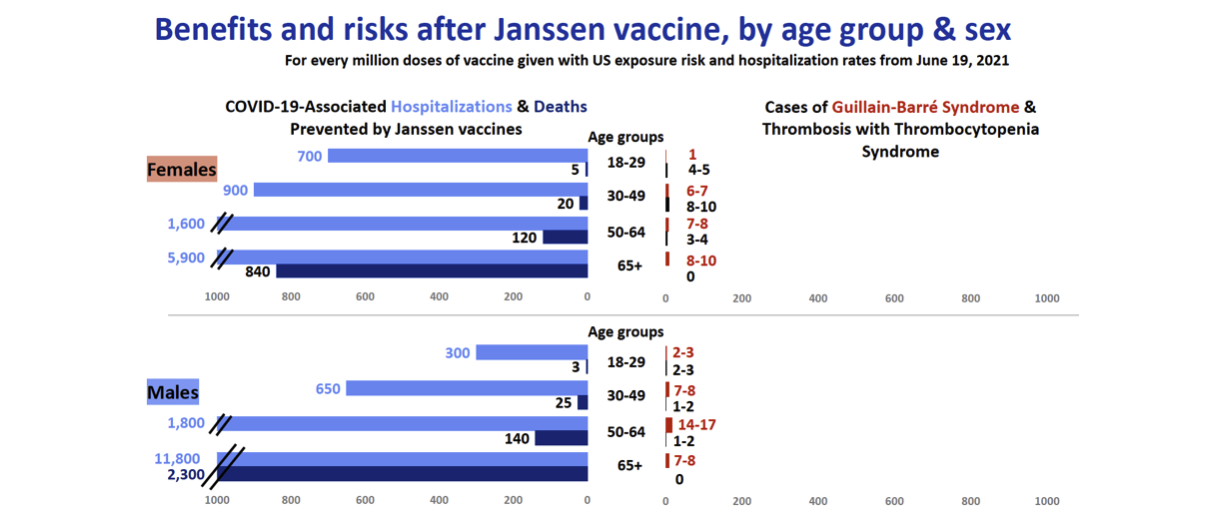
Source: CDC
Research Highlights
Difference in mortality among individuals admitted to hospital with COVID-19 during the first and second waves in South Africa: a cohort study
- Data on SARS-CoV-2 infections were from national epidemiology reports and data on hospital admissions were from DATCOV. DATCOV is an active surveillance system collecting data from all hospitals in South Africa that admitted a person with COVID-19. As of March 27, 2021, 644 health facilities were reporting into DATCOV.
- Authors divided the period of March 5, 2020, to March 27, 2021 into five periods using hospital admissions data (pre-wave 1, wave 1, post-wave 1, wave 2, and post-wave 2). Authors defined the beginning of a wave as five new admissions per 100,000 people and the end of a wave when incidence returned to this level.
- Overall, 23.38% of hospitalized patients died (51,037 people died of 219,265 COVID-19 patients for whom outcome was known). At the peak of the second wave in January 2021, the in-hospital case fatality risk was 29.34% (95% CI 28.95–29.74), which was significantly greater than at the peak of the first wave in July 2020 (21.80% [95% CI 21.39–22.22; p<0.0001]).
- The incidence of COVID-19 admissions also increased at a faster rate during the second than the first wave. The time from five hospital admissions to 15 per 100,000 population in the first wave was six weeks and five weeks in the second wave.
- In-hospital case-fatality risk increased from 17.7% in weeks of low admission (<3500 admissions) to 26.9% in weeks of very high admission (>8000 admissions), potentially reflecting overwhelmed hospital capacity.
- Comparing characteristics of people admitted during the first and second wave, individuals in the second wave were more likely to be: aged 40 or older, of mixed race, and admitted to public rather than private hospitals. Patients admitted during the second wave were less likely to be of Black or Indian race and less likely to have a comorbid condition.
- Limitations of the study included lack of information about out-of-hospital deaths, inability to account for differences by province or district and high proportion of missing data, especially for race (32%) and comorbidities (22%). Authors also were unable to adjust for changes in national COVID-19 restrictions, which may contribute to residual confounding. A lack of individual-level SARS-CoV-2 lineage type data was another limitation. More hospitals started reporting to DATCOV in October 2020 after the peak of the first wave (July 2020) which may also have underrepresented hospitalizations and deaths during the first wave. Large differences (e.g., in age, comorbidities, obesity) between people who died and those who survived or were not infected during the first wave may have resulted in a healthier population being infected during the second wave. This may have lowered the mortality rate during the second wave.
Household Transmission of SARS-CoV-2 from Children and Adolescents
- Researchers followed 224 children between 7-19 years of age who tested positive for SARS-CoV-2 after exposure during an outbreak at an overnight camp (hereafter referred to as ‘index cases’). These children returned home to 194 households and 526 household contacts.
- 198 (88% of) index cases had symptoms due to COVID-19, 141 of which (71%) developed symptoms after returning home. The majority of cases (79%) occurred in households where the index patient became symptomatic after returning home.
- Transmission occurred in 35 (18%) of 194 households. In those households, the secondary attack rate was 45% (95% CI, 36 to 54).
- 74 (14%) of 526 household contacts had at least one underlying medical condition. Among the household contacts who became infected and who were at least 18 years of age, 4 (10%) of 41 were hospitalized.
- 146 (67%) of 217 index cases reported that they had maintained physical distancing and 73 (34%) of 216 reported that they had always worn masks around contacts at home. Physical distancing and mask use were associated with older age of the index case.
- Among household contacts, the risk of infection was lower among contacts who practiced physical distancing (adjusted odds ratio, 0.4; 95% CI, 0.1 to 0.9). The risk of infection was higher among contacts who had close contact with an index case than among those with no/minimal contact (adjusted odds ratio, 5.2; 95% CI, 1.2 to 22.5). The risk of infection was higher among parents of index cases when compared with siblings (adjusted odds ratio, 2.3; 95% CI, 1.1 to 4.7). The risk of transmission was not associated with age of the index case.
- Limitations include difficulty in disentangling the biological effects of age with the effects of behavior and contact patterns on risk of transmission even when multivariable models are used. It is possible that secondary cases arose from contacts outside the household. Secondary attack rates were probably underestimated because testing was voluntary.
Suggested citation: Jones SA, Cash-Goldwasser S, Wu AC and Frieden TR.. In-Depth COVID-19 Science Review August 2, 2021. Resolve to Save Lives. 2021 August 2. Available from https://preventepidemics.org/covid19/science/review/