COVID-19 in Africa: Are reported cases and deaths only the eyes of the hippo?
COVID-19 cases and deaths reported from Africa
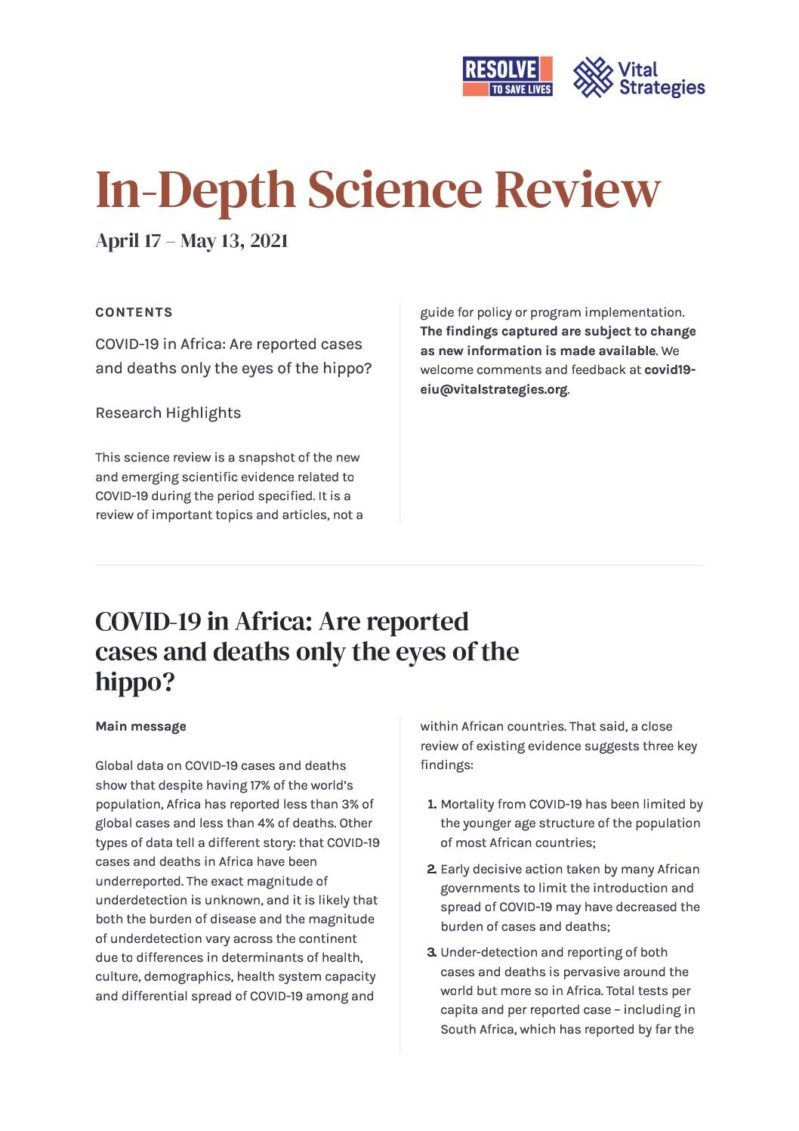
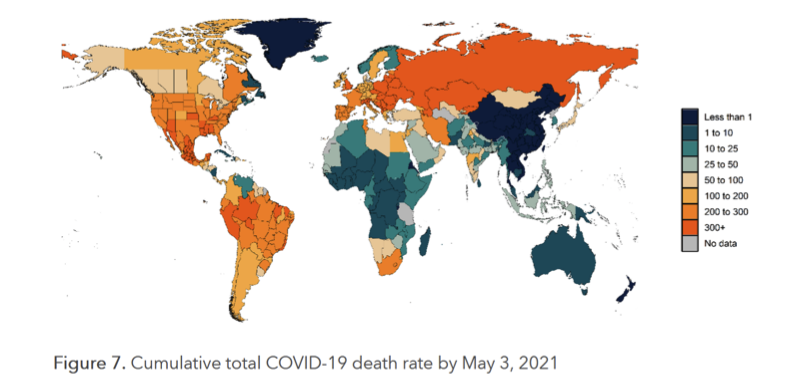
There have been more than 4.6 million cases of COVID-19 and more than 124,000 deaths reported across Africa. These are high counts, but they are relatively low compared to those reported from other world regions. At the beginning of the COVID-19 pandemic, there was great concern about what the pandemic might mean for Africa due to a number of health, demographic and economic factors. These include: a high prevalence of infectious (e.g., HIV and tuberculosis) and non-infectious comorbidities (e.g., cardiovascular disease, diabetes, malnutrition); the fragility of many health care systems; the relative inability to shield vulnerable people from infection (many older people live in large mixed-generational households and the risk of transmission within households is high); and challenges implementing mitigation measures for those living in poverty. Early models predicted that Africa would experience high case and death counts. Whereas a tremendous first pandemic wave hit other regions in early 2020, Africa appeared to experience a relatively slow, small first wave. At the end of 2020, many regions, including the African continent, experienced a second wave; in Africa there was a 30% increase in the number of new cases per day compared with the peak of the first wave. In South Africa, a surge of cases and deaths overwhelmed hospitals, similar to the situation in some of the hardest-hit countries in Europe and the Americas. However, when the numbers reported across the globe for the entire COVID-19 pandemic are totaled, despite having 17% of the global population, Africa has accounted for less than 3% of global confirmed cases and less than 4% of global deaths.
Source: Our World in Data
Why have there been relatively few COVID-19 cases and deaths reported in Africa when compared with other regions?
There are three leading explanations for why there have been relatively few COVID-19 cases and deaths reported in Africa: true differences in risk, the effects of mitigation measures and underdetection.
- Is the risk of death from COVID-19 lower in Africa?
First and foremost, age is the single strongest predictor of the risk of death from COVID-19. Estimates of age-specific COVID-19 fatality rates suggest that someone who between 65 and 74 years of age is over 600 times more likely to die of COVID-19 than someone who is under 35 years of age. Africa has a relatively young population, with a median age of 19.7 years for the continent, whereas in the U.S., for example, the median age is 38.6 years. There are an estimated 1.05 billion people 60 or older in the world; only 73 million (7%) of them live in Africa.

Source: United Nations
To explore whether population age structure may explain the difference in reported COVID-19 deaths, one may apply age-specific COVID-19 case fatality rates to regional population age structures. A preprint analysis that used this approach estimated that the rate of COVID-19 deaths in North America would be four times higher than the rate in Africa. As of May 10, 2021, approximately 0.1% of North America’s population had reportedly died from COVID-19 compared with approximately 0.01% of Africa’s population—a ten-fold difference. Also of note, studies suggest that given contact with a COVID-19 case there is variation in susceptibility to infection by age, with children less likely to be infected than adults. That children comprise a relatively high proportion of Africa’s population may reduce transmission and thereby reduce case counts. However, this factor alone cannot explain the vast differences in incidence or cumulative case counts among regions.
There have been other hypotheses proposed to attempt to explain Africa’s relatively low case counts. Climate is invoked as a potential pandemic-mitigating factor: warmer, wetter weather could reduce transmission of SARS-CoV-2. However, many countries with tropical climates are low- or middle-income and thus may have reduced capacity to detect cases, as well as a range of factors (including younger population age structure) that may also reduce COVID-19 burden. Multiple studies suggest it is likely that factors other than climate are more important drivers of COVID-19 spread. Other hypotheses include: population genetic factors; cross-protective immunity due to coronaviruses other than SARS-CoV-2; differences in population mobility; differences in population density; increased time spent outdoors; and the list goes on. As of this writing, there is not strong evidence that any of these factors sufficiently explain the comparatively low case rates reported from Africa.
- Have African countries achieved greater success in mitigating the spread of COVID-19 compared to countries in other regions?
As we previously wrote, many African countries acted early to implement public health and social measures to prevent disease transmission. The first COVID-19 case in Africa was reported in Egypt on Feb. 14, 2020, just two weeks after the World Health Organization (WHO) had declared the outbreak a public health emergency. On Feb. 22, an emergency meeting involving the African Union, Africa CDC and ministers of health from across the continent was convened to develop and endorse a continental strategy for controlling COVID-19 in conjunction with WHO. As of April 1, 2020, there were approximately 6,000 confirmed cases across all of Africa, and most countries had fewer than 100 cases. Despite this low level of detected cases, most African countries had stringent measures in place including school closures, workplace closures and travel restrictions.
Countries were also able to leverage their extensive experience controlling other epidemics. For example, Rwanda had designed comprehensive infection control plans after the 2014-16 Ebola epidemic in West Africa that included intensive monitoring at borders, efforts that were expanded to include screening for SARS-CoV-2. These rapid responses may have contributed to lower levels of disease being introduced—slowing the initial spread of COVID-19 on the continent. South Africa adopted a model COVID-19 alert level system to inform the type and duration of mitigation measures needed to control the spread of COVID-19 while minimizing secondary harms to the extent possible. This system guides the implementation of mitigation measures using several criteria including the amount of SARS-CoV-2 transmission, health system capacity and socioeconomic impacts of mitigation measures.
- How much of a problem is COVID-19 underdetection in Africa?
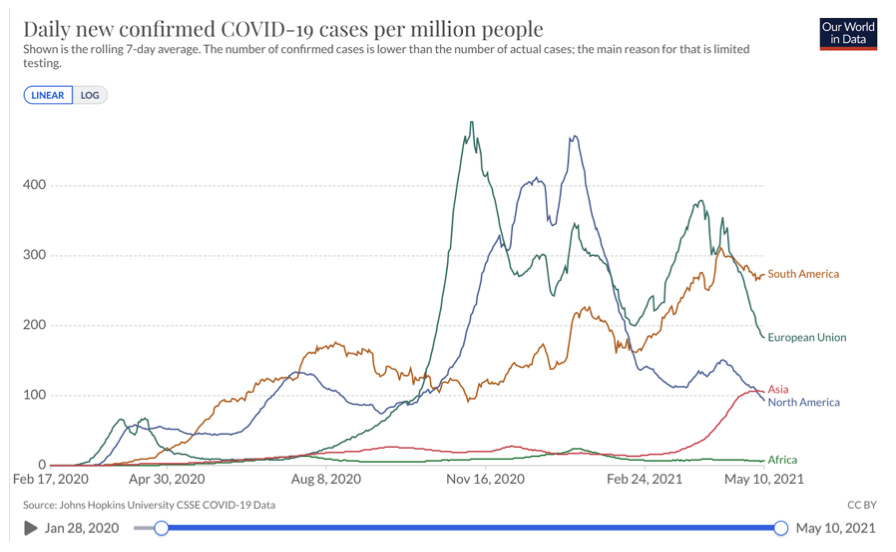
Many factors may influence capacity to adequately detect COVID-19 cases. First, as we previously wrote, COVID-19 case counts are highly dependent on the quantity of COVID-19 testing. The rate of COVID-19 tests per population continues to be lower in Africa than most other parts of the world. For example, by May 7, 2021, the Our World in Data database showed that as a 7-day rolling average there were more than 14 tests performed per 1,000 population in the United Kingdom, 2.7 per 1,000 population in the United States, 1.3 per 1,000 in India and Colombia, but only 0.4 per 1,000 population in South Africa and less than 0.1 per 1,000 population in the Democratic Republic of Congo. As others have cautioned, because of limited testing, relatively lower rates of COVID-19 cases and deaths should not be misconstrued as evidence that COVID-19 has not had an impact in Africa. A study of data from Madagascar suggested that fewer than 1% of COVID-19 cases were detected in the country through August 2020, in part because of limited testing capacity and insufficient access to health care.
Source: Our World in Data
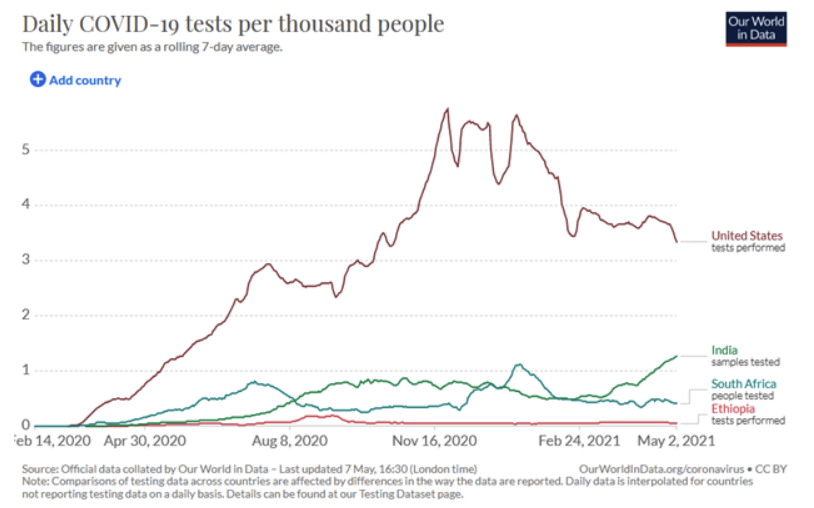
Over the past 14 months, COVID-19 testing capacity expanded quickly but unevenly in Africa, which suggests that the extent of underdetection of cases likely varies by location. In early February 2020, only three African countries were able to perform COVID-19 tests. In April 2020, the African Union Commission and Africa CDC, with support from Resolve to Save Lives and others, launched the Partnership to Accelerate COVID-19 Testing (PACT) to strengthen COVID-19 testing capacity; by July 2020 all 55 African Union member states were conducting COVID-19 testing. The number of tests conducted per month increased more than five-fold, from about 600,000 in April to about 3.5 million in November. However, six of 55 countries accounted for more than 62% of all COVID-19 tests reported by African states in 2020. These same countries accounted for 70% of reported cases (South Africa, Morocco, Ethiopia, Kenya, Egypt and Nigeria). In contrast, one third of countries reported fewer than 10 tests per COVID-19 case, which corresponds to a cumulative test positivity rate >10%. When compared against WHO’s recommended threshold of less than 5% test positivity, this suggests an inadequate level of testing.
Access to testing may also be lower in more remote areas. Authors of a study on the spatial distribution of COVID-19 cases in Niger noted that limited access to testing and awareness of COVID-19 made it less likely that COVID-19 cases would be detected in remote areas, which could lead to overestimates of the extent to which the burden of disease was clustered in the capital region. Rapid diagnostic tests may be one way to scale up testing, particularly in remote areas with limited resources. However, due to poor reporting systems, results from these antigen tests may not be reported to public health officials for inclusion in case counts, and antigen test sensitivity is lower than PCR testing.
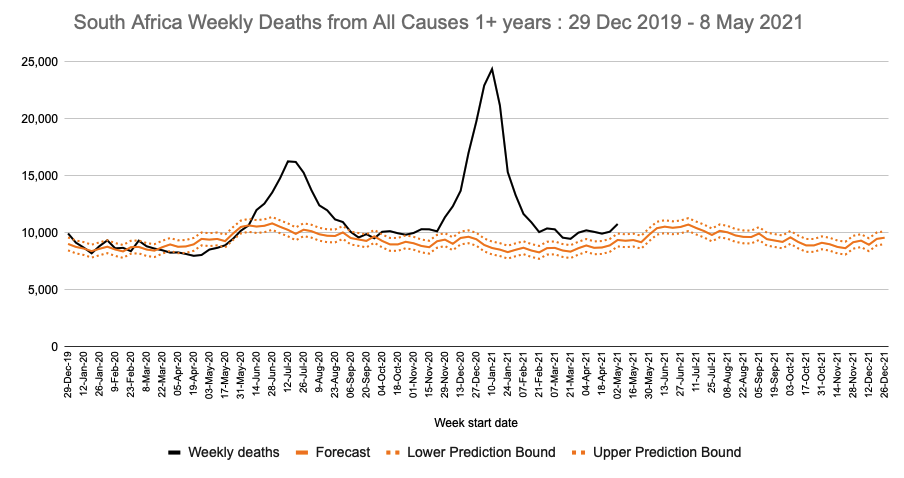
Consistent with limited capacity, early in the pandemic, testing policies in most African countries prioritized testing for those most likely to be positive, such as symptomatic people admitted to hospitals, or travelers entering the country to prevent spread. By April 2021, in most countries testing became available to anyone with symptoms, and an increasing number of countries were offering open testing, including for people without symptoms. Despite an overall trend toward greater availability of testing, there have been temporary declines in testing access or demand in some countries. For example, in late 2020, the Ghana Health Service decided to focus testing on symptomatic patients seeking care at hospitals due to a backlog of samples waiting for testing. Testing rates declined until January 2021, when contact tracing was reactivated in some Ghanaian cities, more people sought care for COVID-19 symptoms at hospitals and demand increased at private laboratories offering testing required for travel.
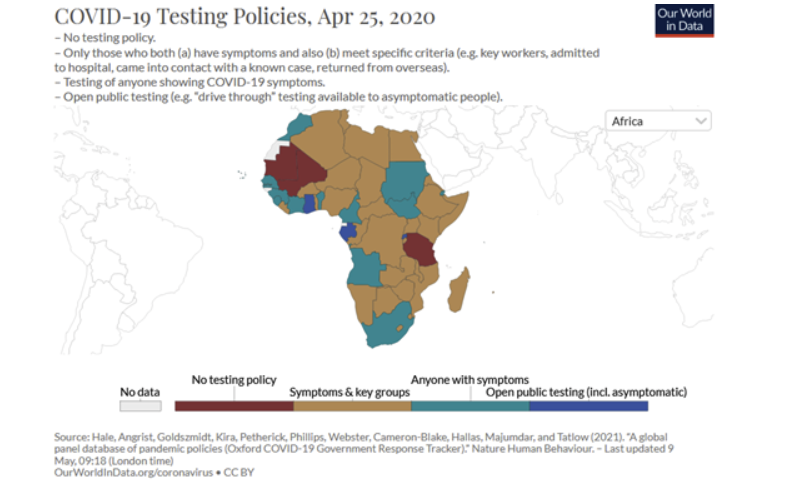
Source: Our World in Data
Challenges in detecting cases are further compounded by factors beyond testing and reporting capacity. First, a significant proportion of SARS-CoV-2 infections may be asymptomatic. Children are more likely to be asymptomatic than adults, and children comprise a relatively high proportion of Africa’s population. Second, when people develop symptoms, they may not seek the care of a licensed medical provider, which can limit opportunities to test for COVID-19. Globally, cultural, economic and logistical factors limit access to health care or care-seeking; some of these barriers may have particularly affected case detection in Africa. Studies conducted in Africa before the COVID-19 pandemic illustrated the extent to which formal care-seeking may be limited. For example, in two urban areas of South Africa, people with respiratory symptoms more frequently consulted pharmacies than government health care facilities. In Madagascar, national surveys indicated that less than half of people with respiratory symptoms sought formal health care. In rural Kenya, although care-seeking was common among those who fell ill, less than half of care seekers went to formal health facilities and the majority who did had previously sought care elsewhere. If care-seeking is delayed, SARS-CoV-2 viral test results are more likely to show a false negative, since the amount of virus present wanes over time. During the COVID-19 pandemic, additional barriers to care-seeking have included health care facility closures, public health and social measures that restrict access to facilities, additional economic barriers and fear of contracting COVID-19 at a health facility. In addition, concerns about the costs of quarantine may also disincentivize COVID-19 testing. For example, in Kenya, people reported fear of a positive test result as a barrier to testing because those who tested positive were required to quarantine and the costs of quarantine were covered by patients. For any or a combination of these reasons, even testing a majority of those who present for COVID-19 testing could result in the detection of only a small minority of infections.
Considering the possibility of case and death underdetection, what can other sources of data tell us?
Seroprevalence surveys suggest significant under-detection of SARS-CoV-2 infections in Africa
Seroprevalence studies, which test blood samples for antibodies to a pathogen to determine the proportion of people that have been exposed in the past, may provide an alternative measure of the proportion of the population infected in the past. Seroprevalence studies have been used to estimate the true spread of COVID-19 across the globe throughout the pandemic, and may be a particularly valuable tool to assess the situation in Africa given the barriers to detection described above. Indeed, a number of COVID-19 seroprevalence studies have been conducted in Africa; many of the results can be viewed on the SeroTracker website, which tracks the results of seroprevalence studies globally.
Seroprevalence estimates from Africa vary widely, both among and within countries. This may be expected given the heterogeneity in risk between settings and populations and across time, even if seroprevalence estimates are derived by testing the general population. Indeed, a critical factor in interpreting the results of a seroprevalence study is the population that was targeted for testing, as this may limit the generalizability of results. For example, many studies have been conducted using samples from blood donations, but blood donors may not represent the general population. This is for many reasons, including their limited age range and relative good health, that they have physical access to blood donor sites (they are likely to live in urban areas and are not shielding at home) and that there may be economic incentives to donate. For these reasons, the Africa CDC is working to standardize the method of conducting serosurveys in Africa by supporting multinational population-based, age, and gender-stratified serosurveys that use standardized protocol and data collection tools.
A sample of seroprevalence studies from Africa are presented here. These were chosen to represent findings from several different countries and study designs::
- An April 2020 cross-sectional study of 301 adult residents of Addis Ababa, Ethiopia, who had no known history of COVID-19 or contact with a COVID-19 case found that 7.6% tested positive for antibodies to SARS-CoV-2. As of the study date, there had been 28 confirmed COVID-19 cases in Addis Ababa; results suggested that the true number of infections in Addis Ababa was likely much higher than reported cases.
- A January 2021 study of nearly 5,000 blood donors between the ages of 15-69 from four provinces in South Africa, estimated that seroprevalence varied between provinces but was high in each one: Eastern Cape – 63%; Northern Cape – 32%; Free State – 46%; and KwaZulu-Natal – 52%. Researchers used those numbers to estimate that the true number of infections was likely many times higher than the number of cases reported. For example, in Eastern Cape, they estimated that infections may have been underdetected by 15-fold.
- A May 2021 study of 3,000 blood donors between the ages of 15-64 who donated to any of four regional blood transfusion centers in Kenya found that 5.6% tested positive for antibodies to SARS-CoV-2. Researchers used that finding to estimate that approximately 1.3 million infections may have occurred by May 30, 2020; only 2,093 cases had been reported in Kenya by that date.
- A study of 84 asymptomatic health care workers in Blantyre, Malawi, conducted from May-June 2020 found that 12% were positive for antibodies to SARS-CoV-2. Four weeks after the survey, 17 COVID-19 deaths had been reported in Blantyre. Researchers used their findings to estimate that approximately eight times more deaths may have occurred in Blantyre than the number reported, though they recognized that health care workers may be at greater risk of COVID-19 than members of the general population.
- A June 2020 preprint study conducted in Niger State, Nigeria, selected 185 participants who were representative of different age, gender and occupational groups to be tested for antibodies to SARS-CoV-2. Testing revealed an overall seroprevalence of 25% and a seroprevalence of 37% among health care workers. Seroprevalence was higher among males than females and in older age groups when compared with younger age groups, but was similar between urban and rural dwellers. The results of a study with this type of design, in which participants who are representative of the general population are selected for inclusion, may be more generalizable.
There are several other limitations to seroprevalence studies. Antibody tests may not always detect SARS-CoV-2 antibodies that are present, yielding false negative results. To account for this possibility, some studies adjust antibody test results upwards. The accuracy of antibody tests may also differ among populations. This may occur because of the immunologic effects of other diseases such as malaria, as was noted by a seroprevalence study from Benin. Several studies have noted challenges interpreting the results of antibody tests performed in African populations, bolstering the argument that tests should be locally validated. Although some seroprevalence studies have assessed the accuracy of SARS-CoV-2 antibody tests using locally obtained samples, many have not. In addition, antibodies to SARS-CoV-2 may decline after infection. This has led some researchers to suggest that the prevalence of antibodies at a given point in time may not truly reflect all cases and that seroprevalence estimates should be adjusted for the waning of antibodies over time (correcting upwards to account for the people who may have previously been seropositive).
Despite the limitations and caveats that must be considered when interpreting the results of seroprevalence studies, the results of studies conducted across Africa overwhelmingly suggest that many more infections have occurred than have been captured by the number of COVID-19 cases reported.
Excess and other mortality data suggest a larger impact of COVID-19 in Africa
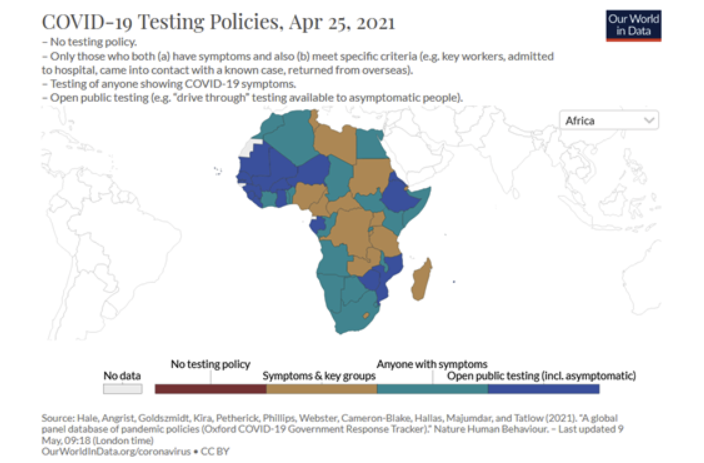
Excess mortality—the number of deaths from all causes during a crisis above and beyond what is expected under “normal” conditions—may be used to estimate the true spread of disease when there are limitations to detecting and reporting cases. As we wrote previously, by capturing both direct and indirect effects of the pandemic on mortality, excess mortality can provide a more complete picture of the burden of the pandemic on a society.
To estimate excess mortality, historical mortality data are used to project the expected number of deaths from all causes during a given period. Excess mortality is then calculated as the difference between the observed and expected number of deaths. As shown below for South Africa, the orange line represents the expected number of deaths based on historical mortality data whereas the black line shows the actual number of deaths per week throughout 2020 and 2021. From May 2020-May 2021, South Africa reported 157,542 excess deaths, or almost three times more deaths than the 54,687 confirmed COVID-19 deaths reported by May 9, 2021. Similarly, data from Tunisia and Egypt suggest that all-cause mortality may have increased by as much as 60-80% during pandemic peaks.
Source: SAMRC
However, mortality data in most African countries are not complete enough to reliably estimate excess mortality. As of 2015, fewer than 40% of deaths were registered in Africa; in some locations COVID-19 has further disrupted existing civil registration systems.
Through a modeling study of global excess deaths (which includes both deaths from COVID-19 and increased deaths from other causes from disruptions to the healthcare and other system), the University of Washington Institute for Health Metrics and Evaluation (IHME) estimated the ratio of reported COVID-19 deaths to actual COVID-19 deaths. Their model suggests that there may have been about three times as many deaths from COVID-19 as reported by countries in Africa. For some countries, the correction was much larger. For example, Egypt reported 13,529 deaths from COVID-19 through early May 2021, but the IHME model suggests that there were actually about 12 times more deaths, for a total of 170,000 lives lost to COVID-19. Even with these corrections, the estimated per capita mortality rate in most African countries is low compared to the United States and many European and Latin American countries. A weakness of this model is that it is based primarily on data from countries with complete mortality registration, which are predominantly high income. This may limit the accuracy of modeled estimates for African countries.
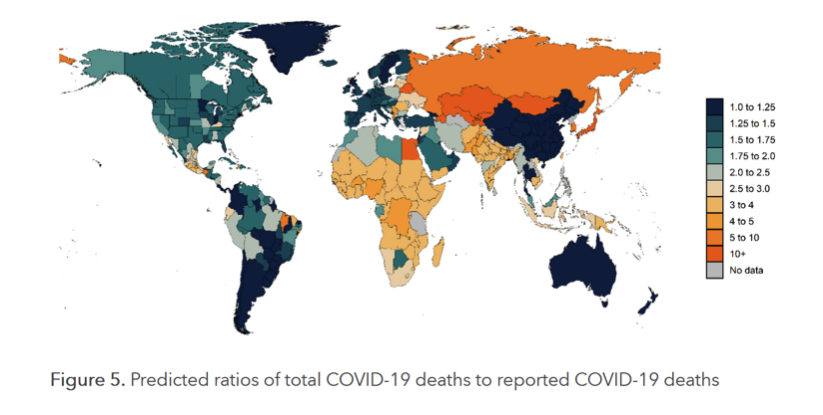
Source: IHME
During the pandemic, besides the excess mortality caused by COVID-19, crisis conditions likely have also contributed to excess mortality in African countries. Due to significant poverty, health system fragility, food insecurity, political instability and heavy baseline burden of other diseases, such as malaria, tuberculosis, and HIV, African populations may be particularly vulnerable to crisis conditions. As we previously wrote, the COVID-19 pandemic and response may have devastating health effects due to impacts on local health systems and, in particular, on essential health services. For example, UNICEF reported that nearly one million Ghanaian children have missed out on routine essential health services, including routine immunizations, while another 1.6 million primary school aged children in Ghana lost access to school meals. Across the continent, income loss remains widespread and continues to worsen, exacerbating conditions that lead to increased morbidity and mortality from a range of diseases. WHO also has reported disruptions in supply chains for essential materials for malaria prevention—such as long-lasting insecticidal nets and antimalarial medicines. These health impacts of the pandemic and response efforts, as well as enormous social, economic, nutritional and educational impacts, are likely to have long-lasting consequences in Africa.
In settings where not all deaths are registered, reports that funerals or burials are occurring more than is typical may also suggest that there is excess mortality. For example, in Kano, Nigeria, grave diggers raised concerns about a sudden three- to four-fold increase in the number of bodies requiring burial in April, 2020. At the time, the only laboratory in the state that offered COVID-19 testing was temporarily closed, which may have allowed COVID-19 to spread undetected. After further investigation, it was estimated that COVID-19 may have caused at least 50-60% of the deaths.
A potentially highly informative, though challenging to obtain, source of data on COVID-19 deaths is autopsy data. Researchers conducted PCR testing for SARS-CoV-2 on a random sample of deceased people of all ages at the University Teaching Hospital morgue in Lusaka, Zambia, during June–October, 2020. Of 364 deceased people with available PCR data, 70 (19.2%) tested positive for SARS-CoV-2. Most of those deaths (51/70; 73%) occurred in the community; none of those people had been tested for SARS-CoV-2 before death. Among the 19 people who tested positive and died in the hospital, six were tested for COVID-19 before death. Although it was not possible for researchers to ascertain whether COVID-19 was the cause of death, data on symptoms before death were obtained for 52 of those who tested positive; the majority of them (44/52) had typical symptoms of COVID-19. This study suggests that it was common for people who died in Lusaka during the study time period to have been infected with SARS-CoV-2 and that mortality from COVID-19 may have been vastly underestimated in Lusaka. Results also showed that a minority of those who died and tested positive were tested before death, including none of those who died in the community.
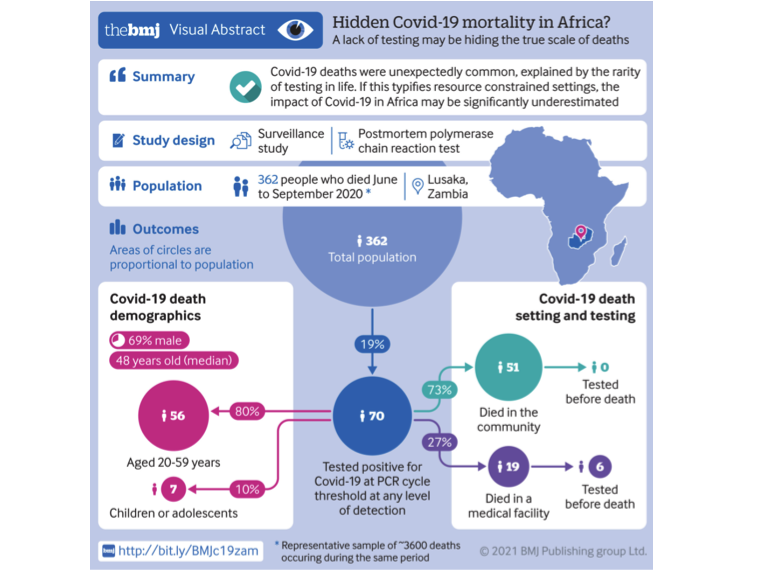
Source: BMJ
Conclusion
Evidence from a wide range of sources suggests that the true number of COVID-19 cases and deaths in Africa is significantly higher than official counts. A better understanding of the true burden of COVID-19 in Africa is critical to guide ongoing efforts to mitigate the spread of, and mortality from, the disease.
In the absence of and until there is widespread vaccination coverage, public health and social measures continue to be an important strategy for COVID-19 control in Africa. However, these measures can be associated with negative social and economic effects that have taken a severe toll on people in Africa over the past 14 months. To minimize negative secondary effects, public health and social measures need to be carefully calibrated to match transmission levels. Detailed, timely data on COVID-19 cases at the subnational level can help determine when measures can be relaxed to mitigate negative impacts, and when more stringent measures are needed. Improving the quality and completeness of data on COVID-19 cases and deaths will require innovative strategies for improving data information systems and further expansion of access to testing.
A more complete account of the burden of COVID-19 in Africa can also inform local and global risk perceptions. Where COVID-19 morbidity and mortality are underestimated, people may view COVID-19 as posing little threat and may be less likely to adhere to and support measures such as physical distancing or wearing masks. Underestimation of the true burden in Africa may reduce the will of, and urgency among, other countries and international bodies to distribute vaccines and other resources to sustain a sufficient COVID-19 response.
Africa may yet face future waves of COVID-19, including with more dangerous variants. COVID-19 surges associated with new SARS-CoV-2 variants are occurring globally, overwhelming health care systems and causing many deaths. Even countries where COVID-19 had previously been relatively well-contained have recently become overwhelmed. Countries with adequate access to vaccines are able to relax public health and social measures to relieve secondary social and economic effects of the pandemic. However, only 1% of the COVID-19 vaccines administered globally have been given in Africa and the extent to which mitigation measures will be needed to combat COVID-19 in Africa over the coming months is unclear. What is clear is that COVID-19 has taken a heavy—and likely largely uncounted—toll in Africa.
Research Highlights
Transient reductions in HIV clinic attendance and food security during the COVID-19 pandemic for people living with HIV in four African countries
(Clinical Infectious Diseases, April 2021)
- Participants were enrolled in the AFRICOS cohort study, which includes both people living with HIV and participants living without HIV (5:1 ratio) in Tanzania, Kenya, Uganda and Nigeria. Researchers compared responses to questions about HIV care and treatment and food security before the pandemic (January 2019-March 2020), during the early stage of the pandemic (May 2020- September 2020) and during the later stage of the pandemic (September 2020-February 2021).
- Compared to pre-pandemic levels, people living with HIV were 36% less likely to attend HIV clinic visits during the early stage of the pandemic (95% CI: 0.45 – 0.91). No significant difference was found between the pre-COVID and late-COVID period.
- Despite the lower clinic attendance in the early COVID-19 period, there were no significant associations between ART adherence and the COVID-19 pandemic. Interestingly, viral suppression was actually 3.3 times more likely in late COVID-19 compared to pre-pandemic. One factor that may have affected adherence levels was that 89% of participants in the pandemic periods reported having access to at least three months of medication supply.
- Results for food security were somewhat similar. People living with HIV were 33% less likely to have had enough to eat in the early COVID-19 period compared to pre-COVID (95% CI: 0.55 – 0.83) and 23% more likely to have had to reduce either the number or size of meals (95% CI: 1.0 – 1.5). No significant differences were found between the pre-pandemic and later pandemic period. Similar results were not observed for participants without HIV (e.g. no significant reduction in food security during early COVID-19).
- Limitations of this study include that participants enrolled in a cohort study of people living with HIV may not be representative of all people living with HIV. Further, the participants who attended a cohort study visit during the pandemic period may not be representative of even the cohort overall (~25% of participants did not attend during the pandemic period). Participants who did not attend were significantly different than those who did. Demographically, they were more likely to be unemployed and to live further from the study site; clinically, they were also more likely to be adherent to their ART but also more likely to have a viral load >1000.
Suggested citation: Cash-Goldwasser S, Jones SA, Bochner A, Cobb L and Frieden TR. In-Depth COVID-19 Science Review April 17 – May 13, 2021. Resolve to Save Lives. 2021 May 14. Available from https://preventepidemics.org/covid19/science/review/