Staying Alert: Navigating COVID-19 Risk Toward a New Normal
COVID-19 risk alert levels
Alert Level 4Very High Risk | Widespread outbreak that is growing with many undetected cases. Take strong measures to limit all contact |
Alert Level 3High Risk | Many cases including community spread, with undetected cases likely. Limit everyday activities to increase safety. |
Alert Level 2Moderate Risk | Moderate number of cases with most cases from a known source. Increase efforts to limit personal exposure. |
Alert Level 1New Normal | Cases are rare and contact tracing can be used to control the virus. Take everyday precautions. |
Purpose
Alert-level systems provide a framework to support clear decision-making, improve accountability and communicate with the public to increase healthy behavior change. This briefing note explains why alert-level systems for COVID-19 are effective, compares models from several countries, and provides the key principles and potential pitfalls to be aware of when developing these systems. It is intended to provide guidance to local, regional and national governments on best practices for alert-level systems, and on how to clearly communicate what behaviors people should adopt in response to changing COVID-19 conditions in their community.
Background
As countries work to find the balance between health consequences and economic disruption caused by COVID–19, they will need to move away from using the “open” versus “closed” dichotomy for society. Risk levels may move up and down depending on spread, containment, and other factors. Governments will need to work with communities to communicate the changing levels of outbreak severity and risk and help people adopt protective behaviors while decision-makers implement policy changes needed to limit the impact of the pandemic.
Color and numerically coded alert systems have been used to communicate risk levels and associated response measures for a variety of threats, including poor air quality, terrorism, internet security, weather events, travel security and other hazards such as volcanoes. No single alert system is appropriate for every setting. However, if designed and implemented well, alert-level systems can be an effective public communication tool throughout all the phases of COVID-19 preparedness and response.
Alert-level system rationale
Risk alert-level systems communicate visually the level of health risk and indicate what measures should be taken at each level to maximize safety. In the highest alert stage, there may be lockdowns that require people to stay home and closures of schools, places of worship and nonessential businesses. As the level of alert is reduced, a stepwise lessening of these restrictions is possible.
When done well, risk alert-level systems promote transparency, accountability and clear communication with the public.
- Transparency: Data supporting each level of the risk alert system should be publicly available.
- Accountability: Evidence-based guidance for each level allows governments, communities and individuals to assume responsibility for their actions.
- Clear communication with the public: Outlining behaviors for each level, and giving the public advance notice of a change in level, can improve protective actions.
Importance of clear risk communication | ||
| Risk communication can help achieve widespread behavior change necessary in crisis response, but it must be done well to be effective. If the public perceives a lack of consistency, competence, objectivity, empathy, sincerity, or transparency the result can be distrust and fear. Conversely, evidence suggests that when the public senses that a response has these positive characteristics, when information is easily understood and communicated through trusted and accessible channels, and when the necessary services are available, people are able to make informed choices, protect themselves, and heed recommended practices. | ||
| Features of clear risk communication | Fundamental questions risk communication should answer for the public | |
|
|
|
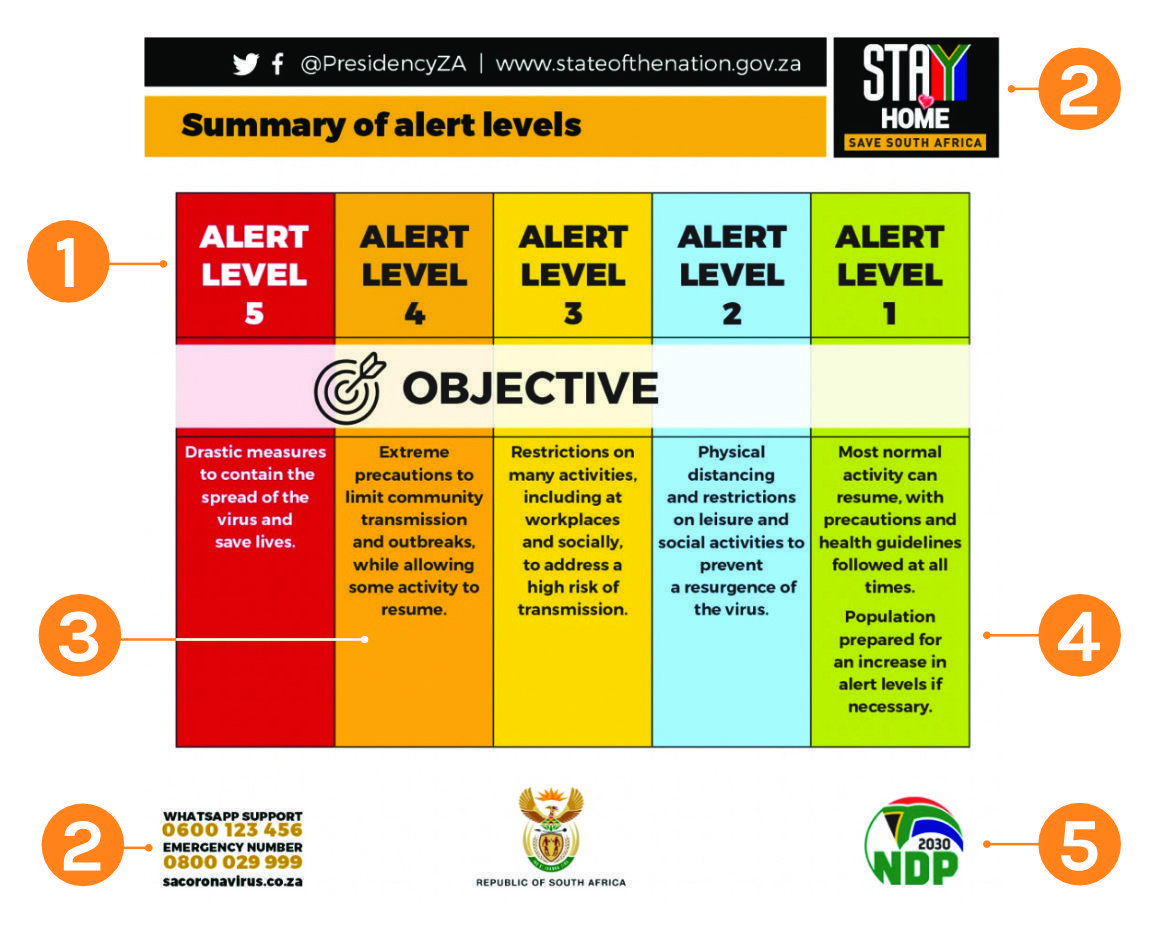
Existing COVID-19 alert-level systems
There are several COVID-19 alert-level systems that can be considered for adoption and adaptation (Table 1). Systems vary with respect to the number of levels, scope, and specificity of guidance provided. Some alert-level systems, such as Singapore’s Disease Outbreak Response System Condition (DORSCON) apply to any disease outbreak and provide messaging to the public. Others, such as the one used in New Zealand, focus specifically on COVID-19 and deliver a risk assessment in addition to messaging on restrictions at each level. The Risk Adjusted Strategy (RAS) in South Africa provides details on how COVID-19 restrictions will be loosened and tightened in each economic sector, using epidemiologic and fiscal data to guide these movements. Some include economic and social indicators when determining the level, such as the state of Utah in the United States.
| Singapore | New Zealand | South Africa | Utah | |
| Schematic | Color only | Number only | Color and number | Color and description |
| Number of levels | 4 | 4 | 5 | 4 |
| Level in May 2020 | Orange | Level 3 | 4 | Red |
| Jurisdiction | National | Town, city, territorial local authority, regional or national level | National, province level | State, counties |
| Level content (types of restrictions) | 3 categories: Nature of disease, impact on daily life, advice to public | 8 categories: Education, | 3 categories: Economic | 3 main categories: General public; businesses and employers |
| Main public health considerations | Transmissibility, situation abroad, domestic situation | Presence/absence of community transmission, clusters, traceability | Epidemiology (e.g., new cases, deaths) vs. health care capacity | New hospitalized patients per day (growth rate), hospital utilization, testing, exposure source |
| Main economic considerations | None | None |
| Currently developing economic (e.g., unemployment) and social indicators |
| Assessment schedule | Unclear | As information changes in any area | Weekly or as information changes | Not specified |
Eight key principles for developing an effective alert-level system
An effective alert-level system incorporates several best practices, including the need to make sure it is clearly communicated.
1. Systems should be easy to understand
A risk level alert system should consist of a small number of levels that reflect risk. Each level of risk should correspond to a set of restrictions or activities directed toward individuals, special populations, or sectors of society such as health care, education, or private businesses.
Using a combination of colors and numbers may be the most intuitive way for the widest array of people to understand the alerts. This visual representation can also increase people’s understanding about what changes in level require in terms of policies and behavior. Systems should be transparent and clear about the rationale behind each risk level and what activities people should do, with additional safeguards for vulnerable people. South Africa’s alert levels are easy to understand and highlight some best practices (see Figure 1).
Source: South Africa
- Using stoplight colors is intuitive
- Leveling system is integrated with fuller communcations effort.
- Level details share both “why” information on risk and “what” the public should do to protect themselves.
- Governments should promote a “new normal” where possible.
- Endorsement by multiple trusted entitites builds public confidence.
2. Systems should be transparent
Transparency of information in times of crisis can improve public trust in government action and strengthen accountability. The content and guidance in the alert-level system should be easily understandable and accessible to the public and to stakeholders who are especially affected. New Zealand’s system has both a detailed and summarized version. In the detailed version, each of the areas covered at the different alert levels, such as public health measures or restrictions on personal movement, has an in-depth explanation. This detailed version may be relevant to some stakeholders, such as hospital administrators who are restructuring services to comply with guidelines. For the general public, the summary table may be enough to give them the information they need to change their actions.
To promote transparency it is critical to:
- State openly the risk rationale, data, and related decision-making to determine levels and to ease or tighten restrictions.
- Make it clear that alert levels are not static and could go up or down depending on disease transmission and associated risks.
- Be consistent in how levels are determined so people can rely on and trust the communication system.
The data used to determine movement between levels (as discussed in more detail below) should be publicly available. This improves the acceptability of the alert-level system. In COVID-19, the epidemiologic situation changes rapidly, with new science emerging every day, and an alert-level system needs to be robust enough to absorb new evidence readily without the need for revamping.
3. Systems should be data-driven
Data should guide recommendations to the general public, specific sectors, and communities about restrictions on movement and activity, as well as extra precautions for individual and community health and safety.
Fundamentally, the material included in an alert-level system needs to be data-driven. This applies not only to decisions on moving from one level to another, but also about the content of the guidance within each level.
In South Africa’s alert-level system, the decision about which nonessential sectors are allowed to open at any level is based on a model accounting for transmissibility of disease within that sector as well as the sector’s economic value and the impact of further continued closure or reopening. Being data-driven also implies that there are clear triggers for each level, making the decision to shift from one level to another an objective one.
4. Systems should be practical
An alert-level system should be detailed enough to be relevant, as simple as possible, and should convey the necessary information. Breaking up the content into categories, as is done in the Utah alert-level system, allows the user to go directly to the section most relevant to them. For example, individuals may look at the general public guidelines to understand how they may participate in controlling transmission (see Figure 2), while businesses can go to sector-specific guidance for detailed information on what the levels mean for them.
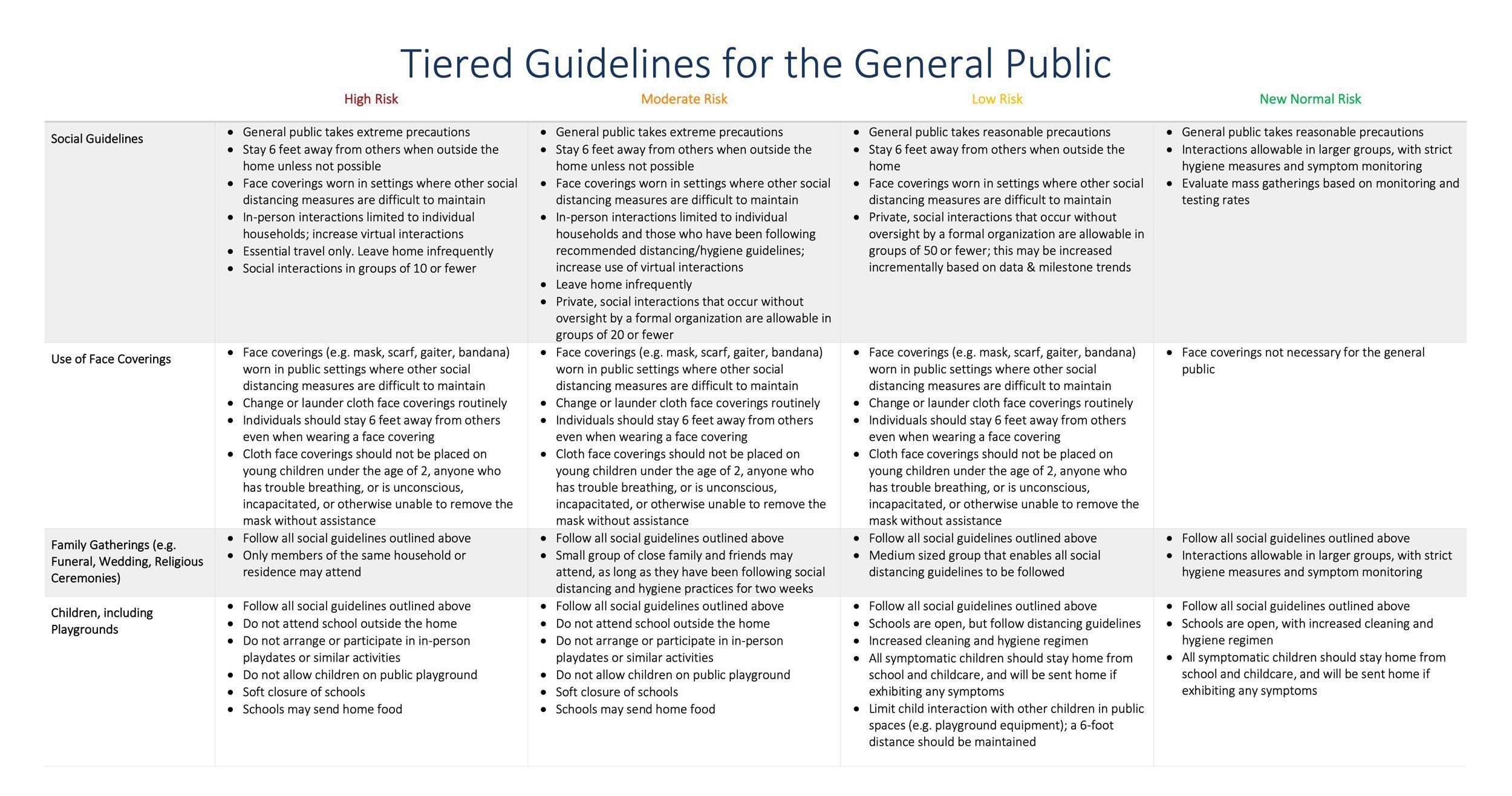
Source: Utah Phased Guidelines for the General Public and Businesses to Maximize Public Health and Economic Reactivation (PDF)
5. Systems should be customized to the smallest geographical area
Each jurisdiction will have to take geographic and cultural factors into consideration when developing an alert-level system. In Singapore, a country of 5.6 million people, the alert-level system is national. In South Africa, a much larger country of 56 million people, the alert-level system can be adapted at the provincial or more granular level.
COVID-19 does not respect borders. Localities must coordinate to avoid promoting movement of people from areas with different restrictions.
6. Systems should be collaborative
When developing an alert-level system, governments should engage a range of stakeholders, including community organizations, and establish a core working group and governance structure, encouraging public discussion and oversight. There should be adequate opportunity for the public and independent experts to discuss and debate the proposal, including triggers, restrictions and protections. There should also be a clear process to evaluate and refine the triggers to move between levels and give authority to a person or committee to make the determination. All branches of government should approve this approach and ensure clear communication of the levels. If different levels are to be used in smaller geographical units, this should be communicated early and built into the system.
7. Systems should be legal, with proper oversight
Some alert-level systems are developed as a pure communication tool, with voluntary guidelines. The health leadership of the government can usually publish such guidance with minimal legal constraints. If, however, the alert levels trigger actions or restrictions required by law, the alert system must have solid legal grounding. In most cases, this will require a law that is approved by the legislature and signed by the executive. If exisiting legislation has already delegated authority to the executive or other body, then regulations or subsidiary legislation may be sufficient. Subnational jurisdictions should confirm that their system complies with national legislation.
Government officials should avoid suspending (or weakening) rights except when absolutely essential, and at the highest emergency levels. When the measures include restrictions of fundamental freedoms and human rights, such as freedom of movement, then the legal measures must include meaningful independent oversight from the legislature, judiciary, independent body, or some combination. This may include a grievance redress mechanism to address disputes. Emergency levels should be reviewed periodically at predetermined intervals, and a best practice is to have an independent group of experts review the criteria, communication and effectiveness periodically.
As restrictions become more strict, they should be accompanied by additional social protections to allow people to comply (e.g., food distribution, utility waivers, paid sick days). If measures include restrictions on international travel and trade, these should be compliant with the International Health Regulations (IHR), including notifying WHO through the IHR National Focal Point.
8. Information should be widely disseminated and made available in appropriate languages
Movement between levels in the alert-level system requires rapid and widely disseminated communication to a mass audience and outreach to specific geographic, linguistic, cultural and ethnic groups within societies. Changes in the risk alert level, whether up or down, must be communicated through mobile devices, mass media, press conferences, websites, social media, etc. In addition to publicizing changes in the levels, authorities should simultaneously make available detailed and transparent information behind the decision-making. In order to have broad awareness, acceptability and adherence, all communication materials should be made available in local languages.
Pitfalls
Alert-level systems do not always work as intended. Implementing a system based on the best practices described above can maximize the possibility of success. One high-profile example of a failed system was the U.S. Homeland Security Advisory System, which was an alert-level system used to communicate the risk of terrorist threats. This system had several problems which resulted in it being dropped. Some of the criticisms of this system and ways to address them include:
- A lack of objective criteria means there is no independent way to determine what the appropriate level should be.
- Solution: use transparent criteria and make decision-making data available.
- Underutilization of levels such that some levels are never used
- Solution: design the system to have meaningful levels that will best communicate to the public the phases of the actual response.
- Overly complex so people don’t understand it
- Solution: develop the system and relevant communication to be able to easily describe the system while providing data and detailed information if needed. Test the system with different groups prior to release.
- Political manipulation such as adjusting threat level for political gain
- Solution: set objective criteria and use publicly available and reported data to adjust the levels. Explain decision-making to the public.
- Lack of public confidence and trust
- Solution: develop a strong communication plan with high-level engagement and frequent updates.
Summary
Alert-level systems can be a core component of effective COVID-19 preparedness and response, and are currently in use in several places around the world. Systems that are developed with consideration for key principles and best practices are more likely to be useful. Every community needs to find a balance, and this may mean allowing economically important activities to begin even before all of the ideal disease control systems are in place—but only if health care workers and the most vulnerable are well protected. If implemented successfully, these systems can help officials lead and communicate effectively with the public, guiding and engaging them on a cohesive response strategy and facilitating resumption of social and economic activities as soon and safely as possible, limiting both the economic and health damage of the COVID-19 pandemic.
Designing and implementing an alert-level system
Several key steps are recommended when developing an alert-level system. The following is a checklist of key actions needed to create and implement the system, along with examples of key sections from around the world.
Our team has developed example alert-level systems for the United States and low-resource settings (see Annex 1 and 2). These examples will be enhanced as COVID-19 information becomes available, experience with such systems is gained and analyzed, and may include indicators that should be monitored, but for which data are not currently available. Note that indicators to be used to determine risk levels do not include all indicators that could be used to analyze and manage the pandemic and the response.
Engage stakeholders and establish a core working group and governance structure.
- This includes high-level political and health leaders who will be the primary group responsible for conveying the alert levels and explaining how they change. It also includes public health, legal and communication experts who can all support best practices and implementation. Generally, alert-level systems are more likely to be followed if they are built with the engagement of government, scientists, businesspeople, community leaders, cultural groups and a wide range of stakeholders who help create the best possible system and become champions for it. It is essential that sound public health principles underlie the categorization, triggers, and implications for actions.
Define the objective, scope and management of the system.
- Clearly define the purpose of the system. What does success look like?
- Identify a lead person/agency and technical leads to design and update the system.
- Determine the the scope of the system in terms of content (e.g., communicate risk, inform sectors and individuals, both, other) and administrative unit for implemenation (national, subnational). National and subnational systems should be be consistent in order to facilitate coherent communication and consolidation of indicators. In some cases, certain geographic areas may have different indicators depending on need.
- Determine when the system will start and end (COVID-19-specific or in place for future infectious disease and/or other threats).
- Develop a process to review and change levels.
- Assign a group to manage the system on an ongoing basis. This includes gathering input which can provide insight and lead to less opposition and more champions of the system as levels go up and down and up again.
Determine the system parameters.
- Determine the number of levels.
- Describe each level (color and description).
- For the description of the baseline/green level, indicate a new/safer normal that is distinct from the pre-COVID situation.
- Identify and monitor data
- Identify indicators and a system to monitor them (e.g., a dashboard).
- Consider epidemiologic risk, transmission and likelihood of control.
- Develop thresholds for indicators to determine levels and when to change levels.
- Change in epidemiologic risk
- Change in ability to manage cases safely
- Change in public health system capacity to support testing, isolation of infected people, contact tracing, isolation and quarantine of exposed contacts
- Identify the public health actions that will be taken at each level
- e.g., Adaptive Response Framework
- Consider the above indicators in the context of economic and social disruption, as indicated in Annex 1 and 2
- Determine how frequently the levels will be updated.
- Be vigilant about monitoring risk.
- Determine change in levels and communication plan for each change.
- Consider the burden of switching too frequently before making any changes.
- Leave room for modification as needed.
Provide clear guidance to support adherence to each level.
- At each alert level, clear guidance should be available to describe the implications of the level on routine activities with specific actions people can take to minimize their risk of infection.
- Consider general approaches to reducing risk.
- Encouraging outdoor activities (e.g., recreation as long as there isn’t crowding)
- Decreasing density of people and number of interactions
- Lower ccupancy
- Staggered shifts
- Working remotely
- Reinforcing physical distancing at work
- Reducing introduction of infected people
- Separating customers from employees
- Screening employees
- Reducing travel risk of employees
- Working in lower transmission geographic areas
- Reducing risk to vulnerable groups
- Keep places clean with routine cleaning and disinfection
- Provide necessary supplies and equipment (e.g., sanitizer)
- Example of general guidance from New Zealand
- Provide detailed guidance for specific groups
- Identify target groups for specific guidance. Groups to consider include:
- General public
- Individuals
- Family gatherings
(e.g., weddings, funerals) - Other large gatherings
- Children
- Outdoor recreation
- Religious gatherings
- Vulnerable/High-risk groups
- Vulnerable individuals
including people over age 60 - Households with vulnerable individuals
- Interacting with vulnerable individuals
- Vulnerable individuals
- Businesses/Workplace
- General employer guidance including cleaning and employer monitoring for symptoms
- Restaurants and bars
- General retail and essential retail (i.e., grocery, pharmacy)
- Entertainment/public venues (e.g., concerts, sporting events, museums, other)
- Personal services
(e.g., hair, nails, tattoos, spas) - Home repair
- Fitness/gyms
- Day care and schools
- Hospitals
- Other health care facilities including dentistry
- Hospitality and tourism
- Travel and transport
- Conduct an analysis to determine the sectors that can open using three key considerations:
- Risk of transmission
- Sectors with lower risk of transmission can open first. Includes places where risk can be mitigated easily.
- Consider the following for each sector (adapted from South Africa)
- % of employees who can work remotely or out of doors
- % of workforce that is older than 60 or vulnerable
- % of workforce in high transmission locations
- Ability to physical distance 6 feet (2 meters) or more at work
- Ability to provide masks to all employees
- Ability to screen all employess
- Ability to isolate all employees
- % of employees who use public transportation
- % of employees who must cross a state, provincial or international border to work
- Consider the following for each sector (adapted from South Africa)
- Sectors with lower risk of transmission can open first. Includes places where risk can be mitigated easily.
- Impact of continued closing on the sector
- Sectors that will irreversibly close or fail should be prioritized to open.
- Economic value of the sector
- Higher value sectors should be prioritized to open.
- Of these, risk of transmission is most important. Places with high risk of transmission that cannot be mitigated should not open, regardless of impact or economic value.
- Risk of transmission
- General guidance on what to open when
- Always open
- Essential services
- Essential retail (e.g., grocery, hardware, pharmacy)
- Hospitals and emergency facilities
- First to open
- Lower risk businesses
- Restaurants with takeout
- Outdoor recreation
- Day care
- Next to open
- Higher risk businesses with modifications
- Schools
- Restaurants dining in
- Last to open
- Bars and tourism
- Conferences and conventions
- Entertainment venues:
movie theaters, concerts, sporting events
- Always open
- Develop specific guidance which includes:
- Sector-specific best practices to prevent transmission
(e.g., hygiene, cleaning, masks) - Modifications to typical practice (e.g., reduce occupancy, telework, takeout food only, redesigned settings, prohibited behaviors)
- Clear directions on what is allowed/not allowed, open/closed
- See examples from Utah and New Zealand
- Sector-specific best practices to prevent transmission
Develop implementation package
- Key communication pieces
- Create simple tools, templates, documents and key messages.
- Create summary and detailed documents describing alert levels for a variety of audiences (i.e., government officials, general public).
- Create translated versions relevant to target populations.
- Develop a website with up-to-date information on the alert-level system.
- Rollout plan
- Develop a communication plan for the initial release of the alert-level system.
- Include media and community engagement.
- Ongoing updates including changes in levels
- Develop an ongoing communication plan.
- Include alert-level updates in the existing system for situational updates
(e.g., press briefings, written updates).
Download Resources:
-
Staying Alert: Navigating COVID-19 Risk Toward a New Normal
(621.93 KB)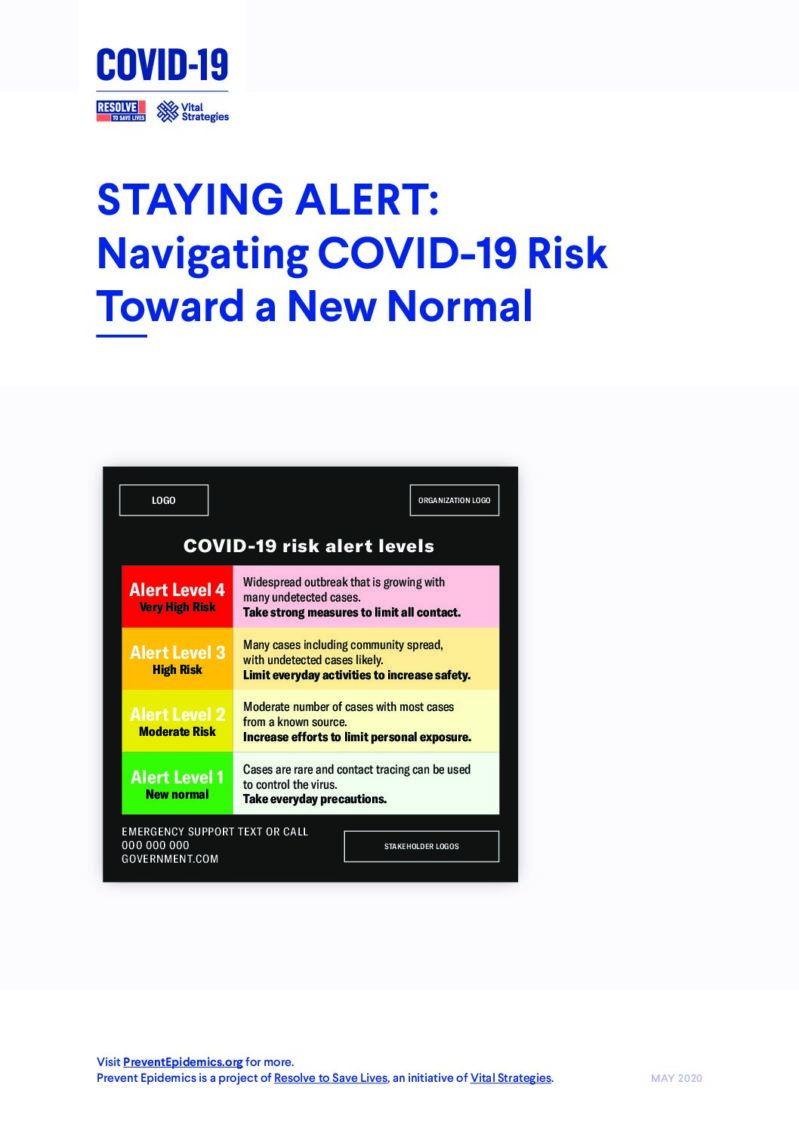
-
Staying Alert | Annex I: COVID-19 alert-level system in resource-constrained settings
(1.19 MB)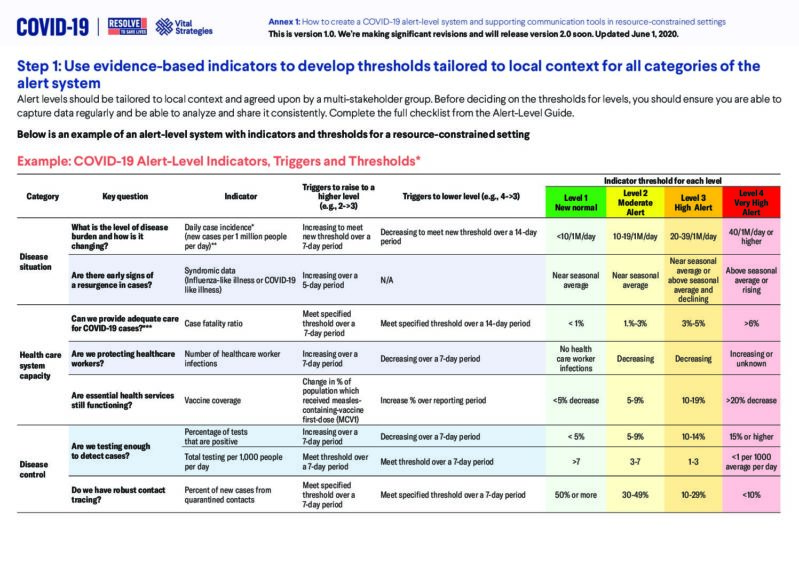
-
Staying Alert | Annex II: Example of an alert-level system
(1,016.34 KB)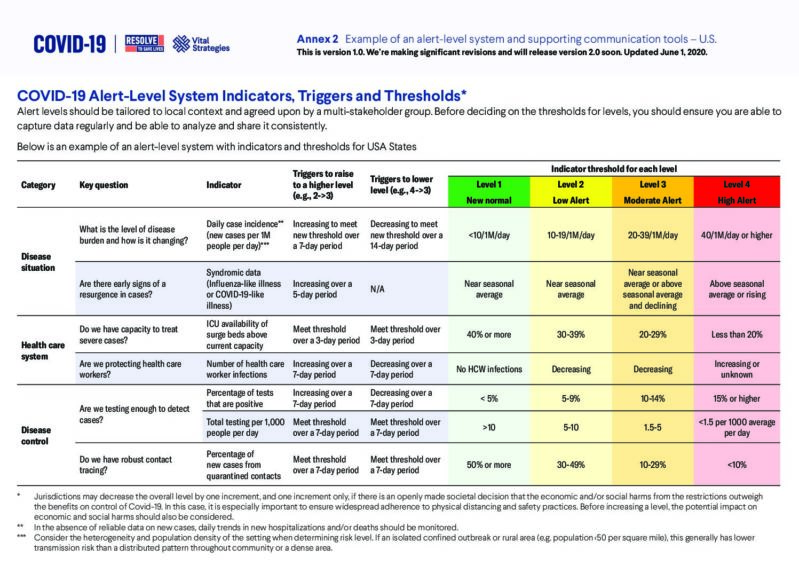
-
Staying Alert | Executive Summary: Navigating COVID-19 Risk Toward a New Normal
(230.73 KB)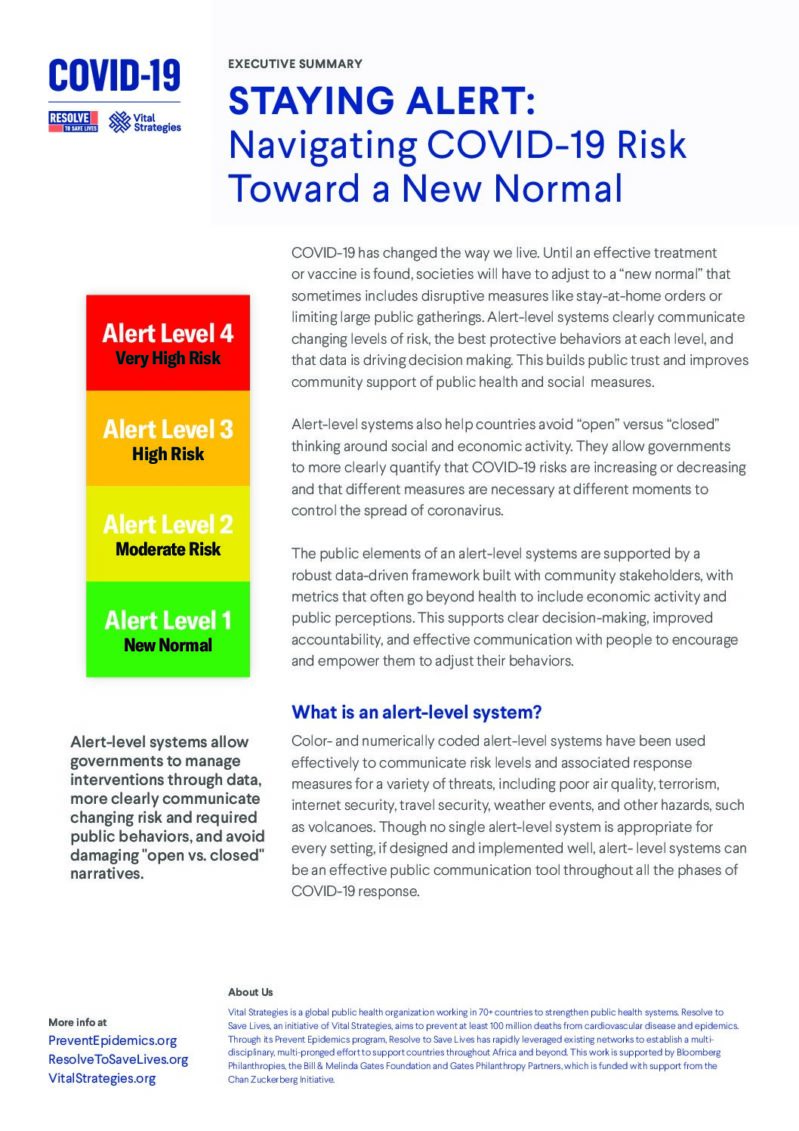
-
COVID Alert System Protects Health, Promotes Economic Growth and Reduces the Risks of Reopening During the COVID Pandemic
-
Rester Vigilant | Résumé: Gérer les risque liés à la COVID-19, Vers une nouvelle normalité
French
-
Permanecendo Alerta: navegando pelo risco da COVID-19, rumo a um novo normal
Portuguese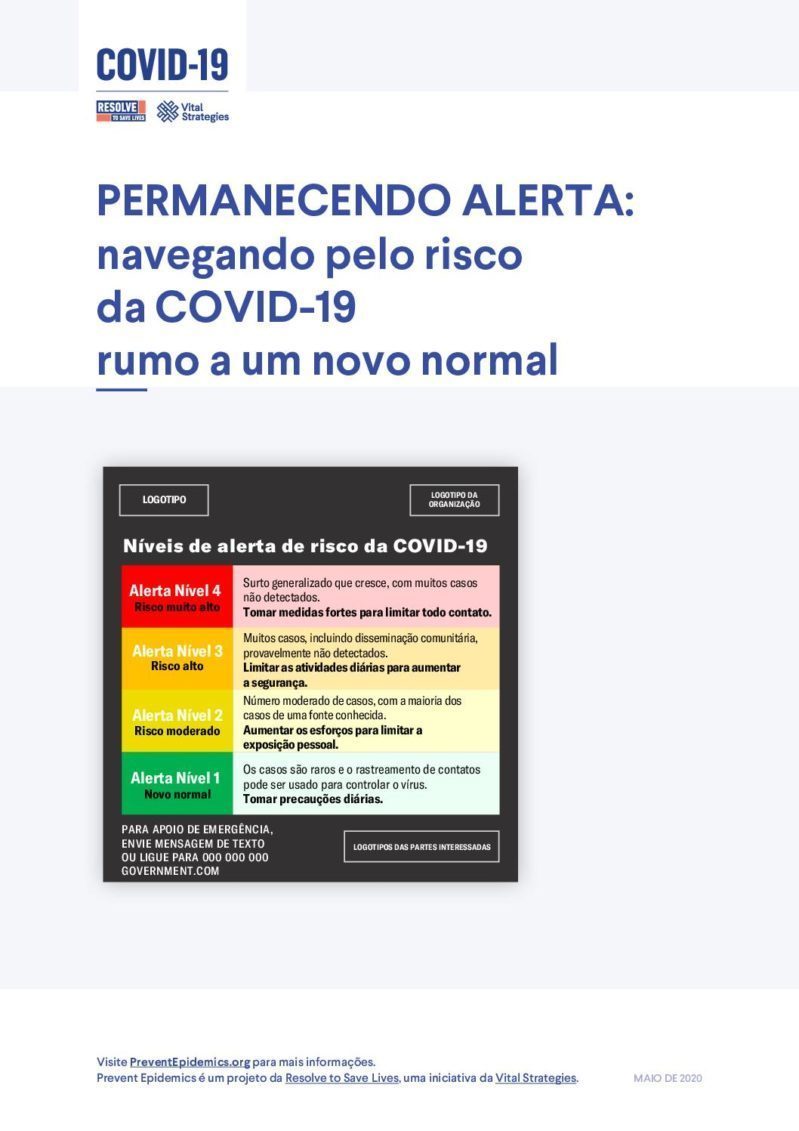
-
Permanecendo Alerta | Resumo Executivo: navegando pelo risco da COVID-19 rumo a um novo normal
Portuguese