Executive Summary
Within months of emerging1, the novel coronavirus SARS-CoV-2 had circled the globe, forcing much of the world’s population into hiding2 and shutting economies and travel3. This withdrawal slowed the explosive spread of the virus to “flatten the curve” of new infections.
But sheltering in place is just a strategic retreat. We’re trapped in our homes, wrapped in our fears, isolated in our stressed hospitals—and in order to go back out, we need to box the virus in.
Many thoughtful approaches for responding to Covid-19 have been proposed.4,5,6,7,8 We benefit from these contributions, as we do from the experiences of states and cities around the country and nations around the world that are responding effectively to the pandemic.
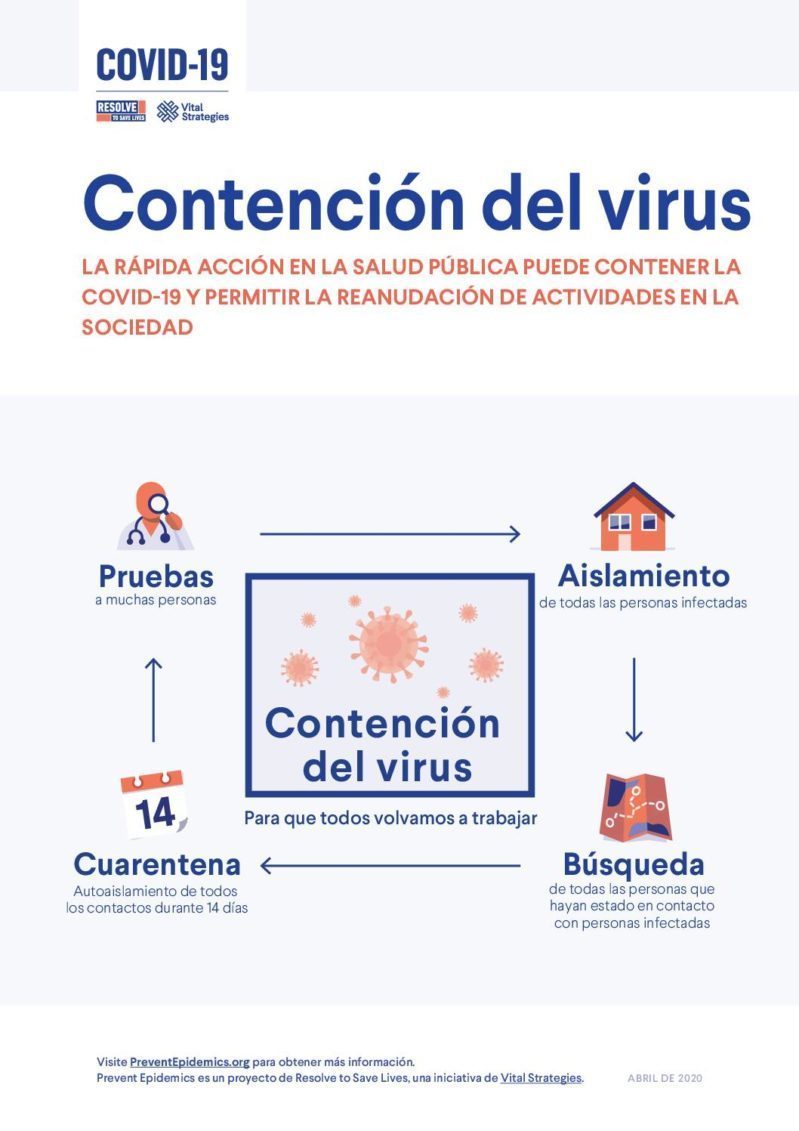
Based on this shared knowledge and drawing on our own experience in the U.S. and globally, here we detail the next step. After flattening the curve, the next step is to box the virus in by implementing four essential actions. All four are crucial; if any one is lacking, the virus can escape and spread explosively again. Success requires urgent expansion of our public health capacity.
- Expand and prioritize testing. We must make rapid diagnostic tests widely available to swiftly identify newly infected people. This report outlines the priorities for testing and approximate numbers of tests needed in different scenarios. Serological testing, which can guide society-wide decision-making, may also make it easier for immune people to reenter the work force but won’t replace widespread testing for the virus itself.
- Isolate infected people to prevent disease spread. We must support every infected person so the virus stops with them, regardless of the setting. Those who do not require hospitalization but cannot safely be cared for in their homes will need safe and attractive housing until they are no longer infectious. Hospitals must safely care for and isolate patients and reduce health care workers’ risk of infection. And the nation’s 15,000 nursing homes need to take extraordinary action to prevent and stop spread of the virus among their 1.3 million residents.9
- Identify contacts who infected people may have exposed. To get ahead of the pandemic, we must trace the contacts of infected people and warn them of their exposure. Just as governments provide hurricane warnings so people can protect themselves and their families, the public sector must warn individuals who have been exposed to the coronavirus so they don’t spread the infection. For this unprecedented effort, we need to build an army of contact tracers, address the public’s concerns about confidentiality and privacy, and adopt technologies to improve efficiency—although new digital tools are likely to supplement but not supplant traditional public health processes.
- Quarantine contacts. People who came into contact with infected people and may have been infected themselves are the leading edge of the pandemic. We must provide them with wraparound services so they can quarantine at home for two weeks and keep the virus from spreading to others. Although some people can easily stay home and work or attend school remotely, others will require special supports, including temporary housing if requested and required. We must ensure that medical and social services are readily available so these quarantined individuals can be tested and isolated at the first sign of illness.
The physical distancing measures we’ve taken to suppress the pandemic have been hugely disruptive, and we are all impatient to resume economic and social activity. We must reopen cautiously: vigilant of new outbreaks, prepared to shelter again if needed, and hopeful that science will yield new vaccines or treatments. We must also lay the groundwork for a safer, more cohesive response to future pandemics. Until there is a vaccine, we will be stuck until we take rapid steps to box in Covid-19, and only public health can guide us there.
Key Recommendations
-
Testing
- Increase the number of diagnostic tests available
- Reduce test result turnaround time
- Prioritize testing for the groups for which testing will make the most difference in improving outcomes and reducing infections
- Determine if antibodies are protective and expand serological testing
-
Isolation
- Make hotels, dormitories, or other facilities that are safe and attractive available for people who cannot safely isolate in their homes
- Prevent transmission in hospitals by rapidly finding and effectively isolating all infected patients and implementing a hierarchy of infection prevention policies
and programs - Implement wide-ranging prevention and control programs in nursing homes, including physical distancing; close monitoring of residents; restricting access to visitors and nonessential personnel; training staff on infection prevention and auditing their performance; screening staff and residents for illness regularly; and ensuring all staff have paid leave so they can stay home if they are sick
- Adopting similar policies in congregate care facilities and reducing their
populations to a level that is safer for residents and staff
-
Contact tracing
- Massively expand contact tracing capacity at the local, state and federal levels
- Support person-to-person contact tracing to make it more efficient and effective, including through the development and evaluation of supportive technologies
- Support contact tracing by having trusted leaders and popular figures explain why
it is so important for cases to help warn their contacts, and why contacts must quarantine until infection is ruled out
-
Quarantine
- Provide services and support to people so they can quarantine as comfortably
as possible - Provide ready access to telehealth services and care when needed
- Provide services and support to people so they can quarantine as comfortably
-
Prevention
- Invest in public health at the national and global levels to tamp down the Covid-19 pandemic and to reduce the risk of future epidemics and pandemics.
Introduction
In the first phase of the coronavirus pandemic, communities that were unable to box the virus in resorted to basic, but battle-tested, public health social measures such as physical distancing to reduce transmission of the virus, and these measures have slowed its spread. This has come at great cost to economies, but these measures have averted an even more catastrophic loss of life.
Hundreds of countries that have closed their borders and billions of individuals who are shut in their homes are wondering what comes next. This is a public health emergency, and public health can guide the way forward.
Although sheltering in place reduces spread of the virus, it does not alter the underlying conditions that can allow Covid-19 to spread explosively if we resume normal activities. To re-open our societies, we must box the virus in by taking the four necessary actions detailed in this report.
We can measure our progress against specific, measurable targets.10 When we meet these targets, we can begin to gradually lift restrictions, loosening the faucet of normal economic and social activity. Significant deterioration of any of the measures should trigger reintroduction of some restrictions, tightening the faucet of activity until the situation is again under control.11
Having a clear plan does not diminish its difficulty. We need real-time, accurate data to track the virus. The people enlisted to find and respond to cases, clusters, and outbreaks swiftly and successfully must be highly trained and well supervised. Building this system will require leadership and a nationwide effort — the health of our people and the wealth of our economy depend on it.
Countries around the world are responding to the pandemic and we can learn from each other’s experiences. The genius of private industry will make new technologies available to increase the efficiency and efficacy of our efforts.
This moment calls for a clear-eyed appraisal of our circumstances and an evidence-based response. The pathogen, not politics, will set the terms of this battle. To open our society before we’ve boxed in the virus would condemn us to another explosive epidemic, another retreat into our homes, another crushing blow to the economy.
1: Expand and Prioritize Testing
In order to contain the virus and control the Covid-19 pandemic, we need to know who is infected. This will require testing, testing, and more testing.12 We need to increase the number of diagnostic tests available, increase processing speed, prioritize, and expand into serological testing.
With widespread, rapid testing, people who show symptoms can quickly determine if they are infected and isolate to protect their families and communities. Health care workers who become ill can be tested and avoid infecting patients and other health workers. Nursing home residents who become ill can be quickly isolated to avoid spreading the virus to others who are highly vulnerable to severe disease.
The crucial nature of testing
Without prompt, accessible, and well-targeted testing, the virus will open new lines of attack, create new clusters and spread illness, death, and economic dislocation.
There are two types of testing: testing for the virus, which identifies people who have current viral infection and are able to spread disease to others, and serological testing, which identifies antibodies showing that a person has been infected at some point in time. Testing for the virus includes low-volume, point-of-care tests that can be used in health centers and for outbreak control, medium-volume hospital-based testing, and high-volume testing, generally provided by commercial laboratories. There are different tests for different purposes and different contexts, and tests will have different roles at different stages in our efforts to box the virus in and stop the pandemic.
There should be capacity to test every person with suspected COVID-19 disease and particularly all with pneumonia, every sick health care worker, every ill person in nursing homes and other congregate facilities (including jails and shelters), contacts, and people in clusters of disease that could be Covid-19. Ideally, unless Covid-19 isn’t present in a community, testing would cover all patients hospitalized for any reason, any outpatient with symptoms of the disease, people working in health care or other essential roles, and close contacts of confirmed cases. In the suppression phase, testing will help find and respond rapidly to new cases and clusters to facilitate reopening society, as well as conduct ongoing surveillance at nursing homes and hospitals and among essential workers.
Estimates vary as to the precise growth in diagnostic testing that is needed. As of early April, fewer than 150,000 people were being tested each day in the U.S., with backlogs of several days.13 The minimum number of tests that need to be done per day will depend on the stage of the epidemic and number of outbreaks, hospitalization rates, number of cases and contacts identified, and decisions about the frequency and extent of testing in nursing homes, hospitals, and essential services. Compared to mid-April 2020, just meeting the need for the highest priority tests would require testing capacity to increase by a factor of 3, and testing on a wider scale as recommended by some could increase the need by a factor of 30 or more (Annex 1).
Actions to increase testing
The federal government needs to ensure that production of tests meets the need for ongoing, widespread testing. Both public and private labs need to accelerate processing. In addition to testing at health care facilities, communities also need to diversify modes of testing, such as drive-through tests.
Ultimately, we must test even more broadly to learn more about presymptomatic and asymptomatic transmission and establish and then hone a new national surveillance system for the virus. We also need to provide repeat testing of cases and contacts to identify when it is safe for people to return to society. A voluntary registry could be established (for example, using the infrastructure of immunization registries available in every state) to identify people who have recovered or who have antibodies to the virus.
Serological testing?
Serological testing identifies people who have or who have had Covid-19. People who test positive for antibodies, but negative for active infection, may have some level of immunity. If they are found to be protected from repeat infection, they could aid in response activities and return to work sooner than others.
Serological assays tests should be widely available, accurate, rapid, and low cost. These tests have already been developed by researchers, with some receiving FDA approval for emergency use, but have not yet been validated. Serological tests will be negative at the early stages of infection, before antibodies have had a chance to develop, so they need to be performed in conjunction with virus testing for active infection. Although people who recover from infection may have some immunity to Covid-19, the strength and duration of this immunity are still uncertain. Whether antibodies are protective, and, if so, for how long immunity lasts, is one of the most important questions to be answered in the coming weeks and months.
Success story: Germany
 Doctor at a Coronavirus Test Station, Germany Nürtingen
Doctor at a Coronavirus Test Station, Germany Nürtingen
Germany tested large numbers of people earlier than any other European country, and is testing at one of the highest per capita rates in the world by including people with minimal or no symptoms as well as those with more severe illness; the country is also implementing antibody testing.14
Widespread testing with timely results has also been a critical component of successful containment strategies in South Korea, Singapore and China.
2: Isolate Infected People
We must swiftly isolate people with Covid-19 to reduce transmission of the virus and to prevent its introduction into environments at risk for outbreaks. We can stop spread of the virus if we isolate infected people and prevent spread of infections at home, in hospitals where our front-line workers and patients are otherwise at risk, and in congregate facilities where populations are particularly vulnerable.
Challenges
Although many questions about Covid-19 remain unresolved, early reports suggest that intrafamily transmission is a significant source of disease spread, which points to the importance of finding safe ways to isolate infected individuals.15
In the early response to Covid-19, health systems in the U.S. and globally have failed to protect their front-line staff from infection. A preliminary CDC report of Covid-19 cases among U.S. health care personnel showed that at least 10,000 were sickened during two months of the pandemic, and in states with more complete reporting, healthcare workers represented 11 percent of total reported cases in that time period.16
Among those sickened by Covid-19, the elderly and people with pre-existing conditions are at much high risk of developing severe illness. The approximately 1.5 million Americans living in the nation’s 15,000 nursing homes17 are particularly vulnerable. By mid-April, more than 2,500 nursing homes reported cases and more than 3,800 staff and residents had died, a number that has been increasing rapidly.18 In some areas, nursing homes accounted for nearly half of Covid-19 deaths.19 Without extraordinary preventive measures, nearly all such facilities could have an outbreak, killing 300,000 residents or more.
Other congregate facilities that house large groups of people together (including shelters, jails, and prisons) are also at great risk for rapid disease transmission. In Cook County Jail, Illinois, more than 500 detainees and correction officers tested positive by mid-April.20
Actions needed
People with Covid-19 whose symptoms do not merit hospitalization must isolate at home if they can do so safely. But for the one in five Americans who live in a multigenerational household,21 others who share a dwelling with medically vulnerable people, people who are homeless, and those who wish to avoid infecting their family members, isolating at home is not the best option. Each community must therefore make hotels, dormitories, or other facilities that are safe and attractive available for these cases to isolate.
Hospitals must adopt policies to prevent transmission by rapidly finding and effectively isolating all infected patients. The CDC has released detailed guidance for healthcare facilities which include reorganizing services, implementing engineering and administrative controls, optimizing use of personal protective equipment, and implementing measures to safely triage and manage patients.22 No health care worker should get infected.
Nursing homes must also take a wide range of actions to prevent introduction of the virus. Following recommendations from the CDC23 and others,24,25 they should adopt physical distancing; closely monitor residents; restrict access to visitors and nonessential personnel; train staff on infection prevention and audit their performance; screen staff and residents regularly for illness—and ensure they have paid leave so they can stay home if they are sick. CDC has created a checklist of policies to adopt. Further extraordinary action may be required, such as testing all staff and residents weekly or daily and physically separating those who are infected.
Other congregate care facilities need to adopt similar measures and should reduce their populations to a level that is safer for residents and staff.
Success story: Singapore
Singapore has been largely able to protect health care workers from infection thanks to smart and rigorously adopted policies. The country had cause to be prepared: during the outbreak of severe acute respiratory syndrome (SARS) in 2003, health care workers accounted for 41 percent of Singapore’s infections. The country first published an Influenza Pandemic Preparedness Response Plan in 2005, and its hospitals regularly train for this type of scenario. The country also built a stockpile of personal protective equipment sufficient to cover all front-line health care workers for several months. And during the response to Covid-19, hospitals reorganized into modular teams that rotate together, reducing exposure among them.26,27 Experts have also credited health care workers’ scrupulous adoption of surgical masks, hand hygiene, and other standard procedures, which have protected them from infection even under circumstances that otherwise put them at high risk of infection.28 Through April, the country counted only a handful of infections among its health care workers, and most or possibly all of these may have occurred in the community, outside of health care facilities.
3: Trace Contacts
We must rapidly and comprehensively trace contacts of people with Covid-19. When exposed people enter quarantine, they interrupt the chain of transmission, which is key to controlling the pandemic.
Contacts of every case must be identified and notified quickly. For this to occur, a massive expansion of contact tracing capacity is needed. Given the size and mobility of the U.S. population and the extend of Covid-19 spread, this will be a monumental task.
How contact tracing works
Contact tracing is a basic public health activity and an essential tool for epidemic response. Contact tracing can prevent a single case from becoming an outbreak and an outbreak from becoming an epidemic. The idea behind contact tracing is simple. In an epidemic, infection isn’t passed from one person to another in a simple chain; it spreads more as if in a web. If just one chain of transmission in this web is missed, the virus can continue to spread through the community.
Contact tracing is time- and human-resource intensive. It requires conducting detailed interviews with every confirmed or presumptive case of Covid-19, detailing their activities hour by hour through the entire infectious period, and recalling everyone they were in contact with during that time. These contacts must then be contacted, interviewed, and, if needed, tested and, if infected, their contacts in turn identified and contacted.
This process continues until the end of any possible transmission chain has been reached. Additionally, all contacts need to self-monitor and report daily on symptoms and temperature for 14 days after their last contact with an infected person.
Building an army of contact tracers
Some communities have begun building contact tracing operations29; we need a nationwide effort with key roles for federal, state, and local public health as well as many governmental and non-governmental organizations. With a coordinated approach, we can then identify and locate people who have been in contact with those who are infected, support them in quarantine, and offer testing as needed.
Contact tracing is a skill. It requires technical knowledge, people skills, and access to resources to help find, and support, index cases (the patient whose contacts are being traced) and their contacts. Supportive, expert supervision is essential to success.
The number of contact tracers needed in the U.S. will be large – as many as several hundred thousand. The number needed will depend on the number of cases that need to be traced, the efficiency of the process, and the level of participation of patients and their contacts. (See Annex 2.) The number of cases will be determined by the extent to which people shelter in place and physically distance to flatten the epidemic curve, infection control in hospitals, nursing homes, and other places where people congregate, and the effectiveness of the contact tracing process itself.
Building public support
The success of the process hinges on the public’s level of participation. Officials and cultural figures should support this process by explaining why it is so important for cases to help warn their contacts, and why contacts must quarantine until infection is ruled out. Because many people are unfamiliar with the contract tracing process, their fears must be allayed in order to stop the pandemic.
When done correctly, contact tracing addresses confidentiality and privacy concerns while allowing governments to take appropriate protective action. The name of the index case is never revealed to a contact. In certain circumstances, index patients may prefer to notify their contacts directly – but public health must ensure that this has been done correctly and promptly. Cases as well as their contacts must be treated as the VIPs of the program – because they deserve this, because it’s the right thing to do, and because doing so increases the likelihood that the chain of transmission will stop with them.
Accordingly, contract tracing programs should include services for those in isolation or quarantine to make the experience safe and as least disruptive as possible. This may entail providing accommodations if a person’s home circumstances are not safe (such as an ill patient living with vulnerable household members), medical and social services, food, and offsetting lost wages.
Emerging technologies
New and emerging technologies cannot replace traditional contact tracing.30 South Korea and Singapore have integrated mobile phone apps into their contact tracing strategies. The exact results and importance of these strategies is still being defined, and should not provide a false sense of security. It is possible, particularly in crowded locations where spread of the virus has been confirmed (e.g., a workplace or church) that mobile alerts and public maps can help people know that they may have been exposed. Location trackers to identify if a case or contact has left their place of isolation or quarantine are being used in some places, although the acceptability and effectiveness of this approach remains to be determined. If patients and their contacts see the process as punitive, patients who are mildly ill may not come forward and patients who do may not list all their contacts. During the 2014-2016 Ebola outbreak in West Africa, Sierra Leone made the mistake of having police guard contacts in their homes, leading to stigma, social hardship, corruption, under-reporting of contacts, and likely prolonging their outbreak by many months.
Other modern electronic tools can make the traditional contact tracing experience more efficient and effective. These include workflow support, call center technology, assistance finding phone and email contact information for cases and contacts, support to help people with infections remember their contacts and their locations, and support for contacts to monitor their health daily and get help they need. Although these technologies have great potential, they are not yet widely available.
However, digital products that promise to provide individuals with an alert on their phone if they have been in close proximity to an individual who has tested positive for the virus raise privacy concerns and have not yet been validated as feasible, accurate, or useful.
Once we implement comprehensive contact tracing, we can support patients and their contacts and prevent outbreaks from becoming epidemics. Until we have a safe and effective vaccine, contact tracing will be crucial to stopping chains of transmission and enabling us to reopen our society and economy as swiftly and safely as possible.
Success story: Wuhan City, China
In Wuhan, China, there were 1,800 contact tracing teams of five people each at the height of their outbreak, roughly one disease detective per 1000 residents.31 Nationally, China has tracked more than 720,000 contacts, isolating those who became infected.32 This has been critical to stopping the spread of disease. After 11 weeks of near-total lockdown, Wuhan’s ability to reduce local transmission to near zero has enabled it to start reopening its society and economy.33
South Korea and Singapore have also used contact tracing very effectively to stop the epidemic in its tracks.34
4: Quarantine Contacts
To control Covid-19, we must ensure that contacts of people with confirmed or suspected infection are quarantined. This will keep the virus from spreading to others if they develop either symptomatic or asymptomatic infection.
The incubation period for Covid-19 is approximately five days on average, but symptoms can take as long as two weeks to develop.35 Infected people can spread infection to others during presymptomatic or asymptomatic periods. Anyone with symptoms can be contagious.36
Unlike SARS, in which patients became more infectious over the first 7-10 days of illness, patients with Covid-19 have high quantities of virus before symptoms develop and at the outset of their symptomatic illness, and this quantity appears to decrease after the first week of illness. This pattern is both a reason Covid-19 is so infectious and an urgent call to action to ensure quarantine of all exposed people.37
How quarantine works
Quarantining people who have been exposed to Covid-19 for 14 days breaks the chain of transmission. This is more restrictive than shelter-in-place orders for the general population, which permit limited travel outside the home for essential needs such as buying food, obtaining medicine, or receiving urgent health care services. True quarantine entails complete separation from everyone outside the immediate household and, for safety, separation from older and medically vulnerable people within households. No travel outside the home is allowed; food and other necessities must be delivered. This is also different from a community-wide quarantine, more properly called cordon sanitaire, as was imposed to prohibit all travel into or out of Wuhan, China during the peak of that city’s epidemic.
If there are additional exposures during the quarantine period (for example, another family member becomes ill), the quarantine period needs to be extended until 14 days after the latest possible exposure. An emerging best practice is testing quarantined contacts for presence of the virus on two occasions toward the end of their quarantine period and obtaining negative results before releasing them from quarantine.
Support for people in quarantine
Although almost all of the U.S. population has been asked to shelter in place and otherwise observe physical distancing, compliance varies greatly among communities, illustrating challenges adhering to quarantine.38 Some people can easily shift to telework, but others cannot. Many people will experience at least some distress due to the lack of social interaction and fear of possible impending illness.
It is essential to provide services and support to infected patients and people under quarantine so that they will adhere to the requirements. This can include provision of food, laundry, and pharmacy services; supplies such as hand sanitizer, masks, and thermometers; free access to high-speed internet, laptops, and even streaming entertainment and educational services. Students may need specialized support to be able to maintain their coursework.
Other resources to support those in isolation or quarantine include provision of cleaning supplies and trash removal; daily check-in phone calls; and a hotline for counseling, information, social services, and medical support. There needs to be ready access to telehealth services and care if needed, with immediate testing and isolation in the event the quarantined person or anyone else in the household develops Covid-19 symptoms.
Forward-looking governments have provided stipends or government-reimbursed payments from employers to compensate for lost wages, and additional child or elder care for dependents. Because the individual may be living in close quarters with a medically vulnerable person, people in quarantine need to be offered voluntary relocation to a safe and appealing location.
In a well-functioning program, most – and ideally all – new cases arise among contacts who have been quarantined. For this to occur, nearly all cases need to be found, all contacts identified, all identified contacts quarantined, and all quarantined contacts, particularly those with symptoms, tested. This is the essence of the Box It In strategy – creating a closed loop so that each wave of infections results in fewer and fewer secondary infections, boxing in the virus and opening more space in society for safe movement.
Success stories: Singapore, Taiwan, and South Korea
Jurisdictions seeking to successfully manage quarantine activities can look to places such as Singapore, Taiwan, and South Korea, which have established strong support systems for people in quarantine.39 Some governments have set policies to support home delivery services for people quarantining at home, including engagement with neighborhood committees and volunteer groups. In South Korea, provinces and cities designate lodgings or other facilities as “living and treatment support centers” for isolation of individuals with suspected symptoms; this concept can also be used when home quarantine of contacts is not feasible.40
Conclusion
By implementing physical distancing, communities slowed transmission of Covid-19 — but did not change the underlying conditions that enable the virus to spread explosively if normal activity is resumed. In spite of the devastation the pandemic has already caused, it is likely that only a small proportion of the population has been exposed; the vast majority of people remain without immunity to the pathogen. The drastic, life-saving actions we’ve taken were necessary, but amount to little more than hiding inside. We have yet to even begin building our defenses. With strategic, swift, large-scale action, we can get ahead of the virus and take the offensive.
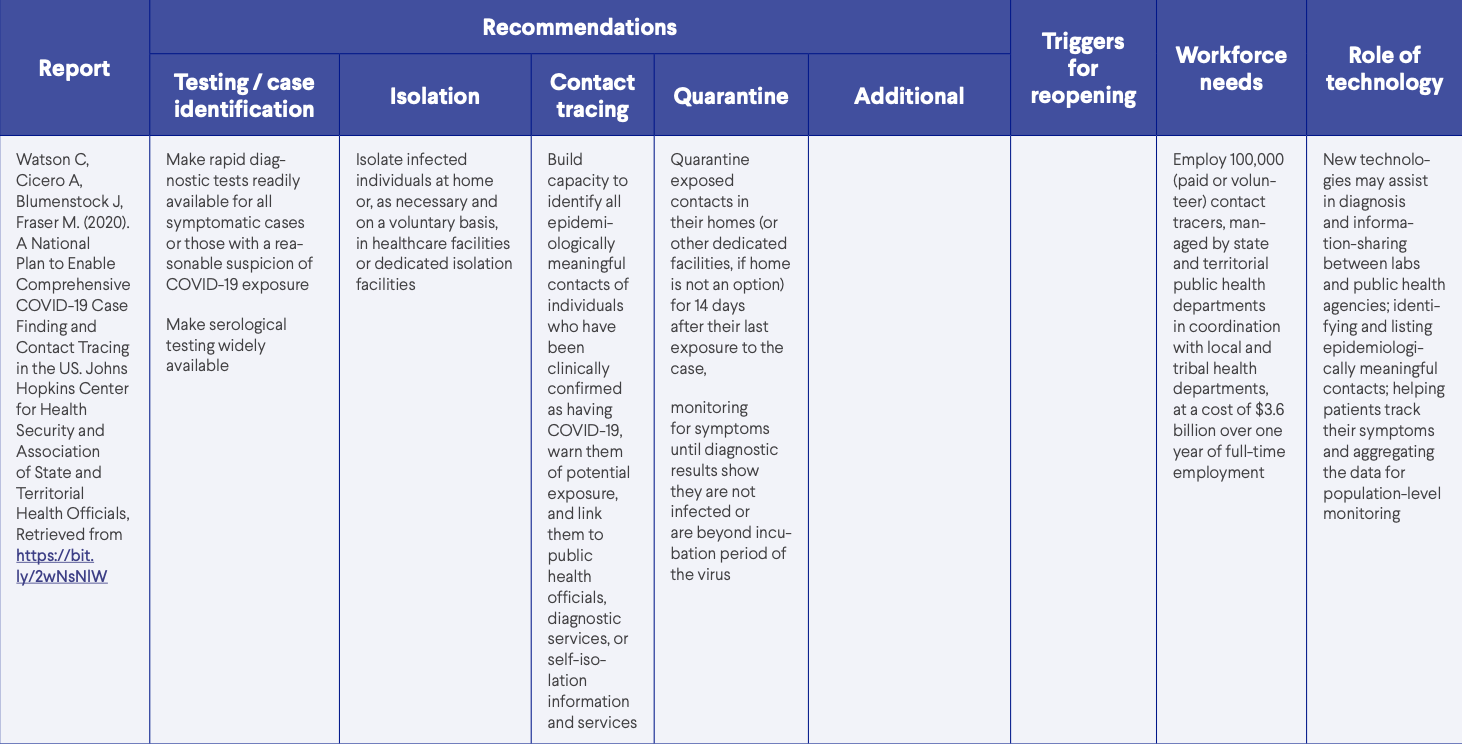
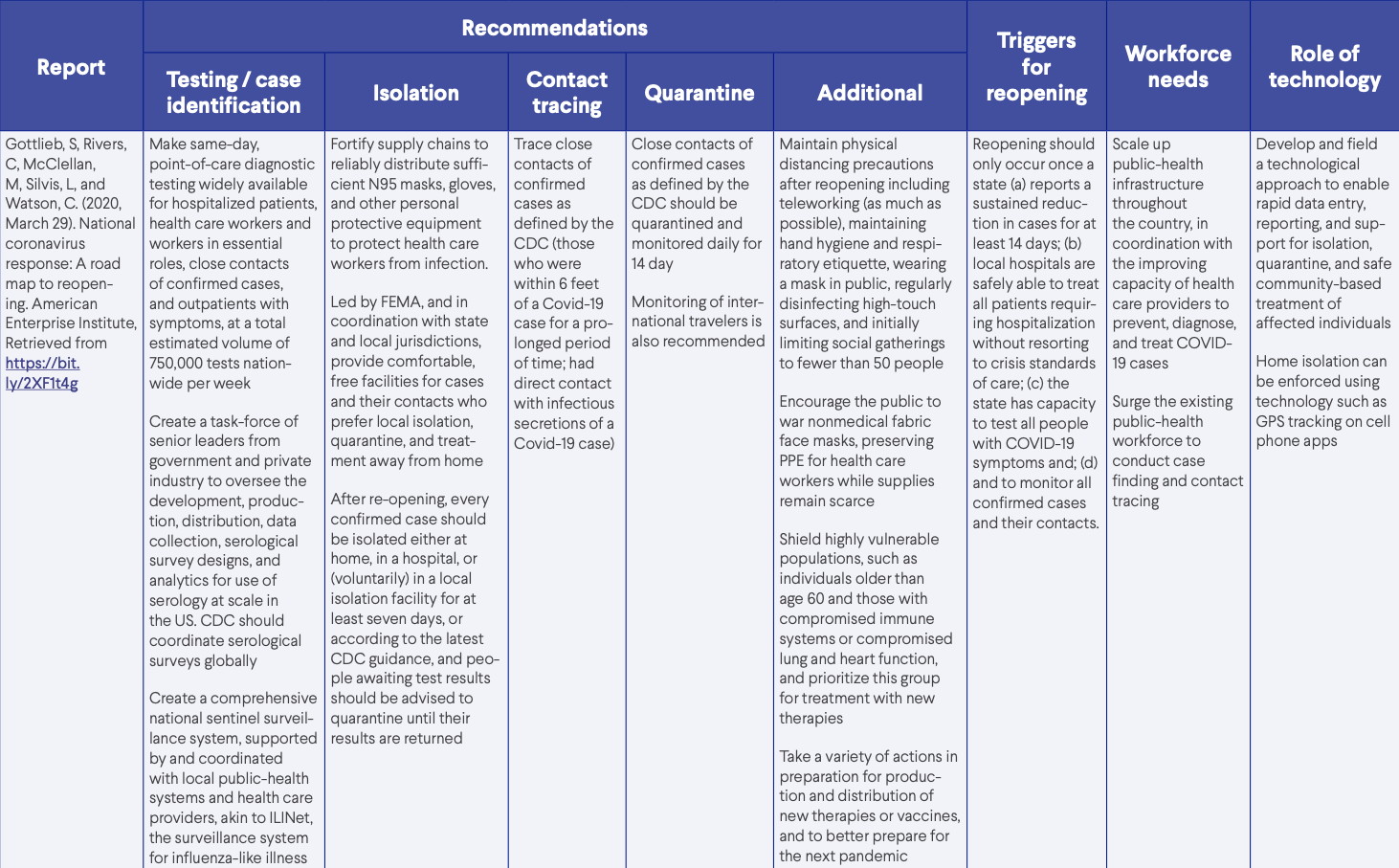
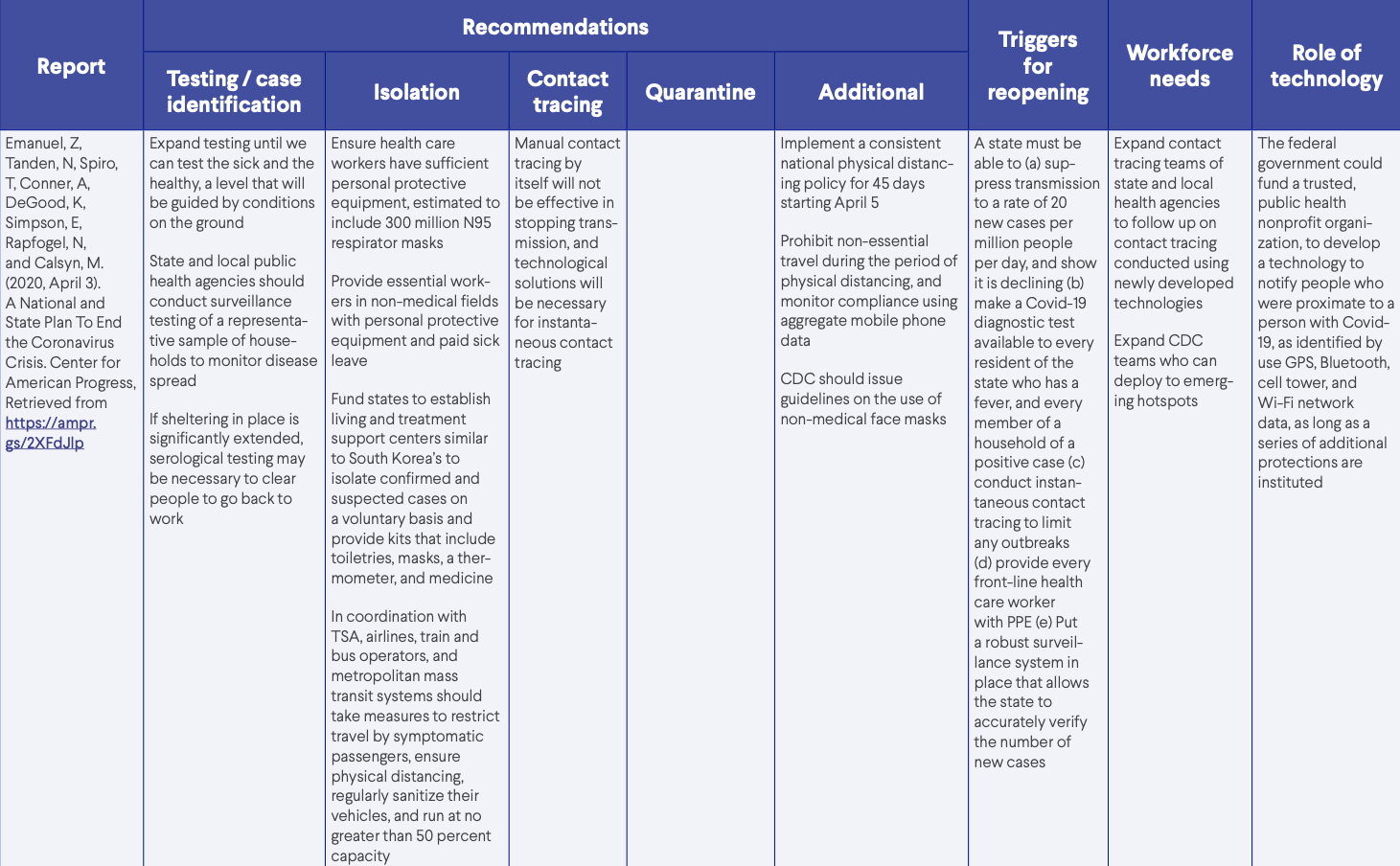
There are important plans and blueprints for responding to the Covid-19 pandemic (Annex 3). This report outlines our next step in the battle, a step which must be guided by core public health principles and practice. The four actions outlined in this report — test, isolate, trace, and quarantine — are necessary to box Covid-19 in, and each is essential for success. If any part of the box is weak, the virus will escape.
We have the resources to build the world’s strongest public health system, one that can curb this pandemic and effectively respond to future ones. In 2018, the U.S. spent just $286 per person on public health activities, but nearly 40 times that – more than $11,000 per person – on health care.41 We must correct this imbalance and invest in protection in the U.S. and globally.
Covid-19 has also illustrated how vulnerable individuals and society are and how important it is to address the underlying health and social conditions that facilitate deadly spread of the virus. We must work to end healthcare associated infections, strengthen primary care, improve health care efficiency including through telemedicine, make medical records interoperable and, when appropriate, accessible for public health action. We must increase individual and community resilience and address not only access to and continuity of care but also the quality of care, the value of care, and the actual health benefit we receive for the public health and health spending we dedicate. All of this will help control Covid-19 and make our society stronger and healthier in the process.
As long as any country is at risk of an outbreak, no country is safe. There are nearly 10,000 life-threatening gaps in disease preparedness worldwide.42 We know where these gaps are, how to fill them, and what this will cost. And we now know, from this painful tragedy, the devastating health and economic costs of our collective failure to prepare. Future microbial threats are inevitable. What’s not inevitable is that we remain so woefully unprepared for them. We must fill the health protection gaps and demand accountability for demonstrating that this is being done.
The Covid-19 pandemic is the most devastating health disaster of our lifetimes. But it is also a once-in-a-lifetime opportunity to repair parts of our health care, public health system, and society that are broken. Public health has the tools to stem this crisis — and must guide us to a new, safer world of stronger global collaboration and solidarity.
Glossary
Covid-19. The name of the disease caused by the novel coronavirus, SARS-CoV-2, and is short for “Coronavirus Disease 2019.” (Source: WHO)
Close contact. A person who has been within 6 feet of a person infected with the virus for a prolonged period of time or has had direct contact with the infected person’s secretions. (Source: CDC)
Contact tracing. The process of identifying, assessing, and managing people who have been exposed to a contagious disease to prevent onward transmission. (Source: WHO)
Containment. Preventing the spread of disease in early stages of transmission through measures such as early detection and isolation of cases, and contact tracing and quarantine. (Source: WHO)
Cordon sanitaire. A measure preventing anyone from leaving a defined geographic area, such as a community, region, or country infected by a disease to stop the spread of the disease.
Coronavirus. A family of viruses that cause illness ranging from the common cold to more severe diseases, such as Middle East Respiratory Syndrome (MERS-CoV) and Severe Acute Respiratory Syndrome (SARS-CoV). The novel coronavirus recently discovered has been named SARS-CoV-2 and it causes COVID-19. (Source: WHO)
Drive-through testing. Individuals remain in their vehicles, and medical staff in protective gear come to administer the swab test and the swabs are sent to a laboratory for testing.
Suppression. Reducing and maintaining low levels of disease transmission through intermittent loosening and tightening of public health social measures, detection and isolation of cases, and contact tracing and quarantine.
Flattening the curve. Slowing a virus’ spread to reduce the peak number of cases and related demands on hospitals and infrastructure (Source: CDC). The objective is to delay the epidemic, reduce the peak and “buy time” to build health capacity.
Isolation. Separating sick people with a contagious disease from those who are not sick. (Source: CDC)
Mitigation. Minimizing the epidemic impact, delaying the outbreak peak and reducing the peak number of cases in order to reduce strain on the healthcare system. Achieved largely through public health social measures and specific treatments and vaccines, if available.
Pandemic. An epidemic that has spread over several countries/continents, usually affecting a large number of people. (Source: CDC)
Physical distancing (previously and sometimes still referred to as social distancing). Measures taken to reduce person-to-person contact in a community, with a goal to stop or slow the spread of infection. Measures can include working from home, closing offices and schools, cancelling events, and avoiding public transportation.
Public health and social measures (PHSMs). Actions, apart from getting vaccinated and taking medicine, that people and communities can take to help slow the spread of pandemic illnesses. PHSMs are also known as community mitigation strategies. PHSMs are among the best ways of controlling pandemic flu when vaccines are not yet available (CDC).
Quarantine. Separating persons who are well and may have been exposed to infection from other persons during the incubation period of an illness. (Source: CDC)
SARS-CoV-2. The name of the novel coronavirus that causes Covid-19 disease. SARS stands for Severe Acute Respiratory Syndrome. Prior to this name, it was called 2019-nCoV.
Serological testing. Testing for antibodies to a pathogen indicating prior infection, which may or may not result in immunity from future infection.
Stay at home or shelter in place. All residents must remain at their place of residence, except for essential activities (buying food and taking care of the health and safety of themselves or anyone in their household, including pets), essential businesses (health care; delivering food, mail, picking up garbage; and maintaining electrical systems etc, and essential government functions).
Annex I
More Testing, Better Prioritized
Until there is much more widespread availability of testing, we need to prioritize. The highest priority are people who should be tested in all communities whenever the virus is present. These include:
- Outpatient, emergency department, and hospitalized patients with suspected Covid-19, and, ideally, all patients who are hospitalized (to prevent spread within hospitals, provide appropriate care, and facilitate enrollment in clinical trials)
- Health care workers with symptoms of Covid-19 (to provide prompt care, prevent further spread in hospitals, and monitor progress reducing risk to health care workers)
- People within clusters of illness consistent with Covid-19, especially if this occurs in a congregate facility such as a nursing home (to identify and stop outbreaks)
- Individuals with symptoms consistent with Covid-19 who reside in congregate facilities such as nursing homes, shelters, prisons, and jails (to prevent outbreaks)
- Contacts of cases
- A systematic sample of outpatients, to track trends of infection
Currently, about one million people in the United States are being tested for active infection per week. Just to meet the highest priority testing needs requires testing approximately three times as many people. The minimum number of tests needed will be even larger if tests aren’t prioritized appropriately either by geography or risk group.
As more resources become available, others can be tested, including essential workers and others in areas such as transportation, food supply, and facility maintenance. Doing so, particularly if testing is conducted on people without symptoms, would require an additional 10-fold increase in testing capacity (approximately 30-fold above current levels). And unlimited testing of various groups, many of whom could require weekly tests, would further increase that need. (This calculation does not account for the number of tests required for a testing-on-demand approach, nor, on the other hand, for the number of people with past infection who may not require testing for the virus itself.) Whether this is a sensible approach remains to be seen.
Serological tests can help better understand the proportion of people who experience only mild or no illness and more accurately determine case fatality ratios; because it seems likely that people with prior infection will have at least some resistance to reinfection, they may be able to more confidently reenter society and aid in reopening efforts.
One interesting proposal has been to test everyone every two weeks for active infection. Although interesting, this proposal is not practical in the near future. The United States does not have enough diagnostic tests, materials, or the capacity to administer that many; even if we did, this might not be the best use of resources.
Laboratory tests are just one part of an ecosystem of care. Accurate testing requires supplies, equipment, safe testing facilities, training and supervision to ensure quality of the sample collection process, improved collection of information on the people being tested (because without complete information, those with positive tests may not be able to be promptly notified of their result), laboratory information systems which connect with health care providers and public health agencies, and more. And, of course, testing is just one of four crucial components to boxing in Covid-19: without isolation, contact tracing, and quarantine of contacts, testing itself will make little or no difference in the spread of the pandemic.
Annex II
Contact tracing is key to safely reopening
Once we have sufficiently controlled the Covid-19 pandemic to allow us to safely start reopening our society and economy, our ability to detect and tamp down fresh outbreaks will be essential to remaining open. Tracing and quarantining contacts of all cases is the best approach to prevent an isolated case from spreading into the community.
We will require thousands of people to properly conduct contact tracing activities at the level needed to effectively close chains of disease transmission and prevent new cases. As noted in this report, contact tracing is time- and human-resource dependent. Exactly how many people we need and for how long will depend on four factors:
- The number of new cases detected per day
- How many people each case may have exposed (e.g., fewer during sheltering in place, more during resumption of usual activities)
- The efficiency of the contact tracing process
- The degree of public support for and participation in contact tracing by cases and their contacts.
The number of people who are infected and the number of people they were in contact with while potentially infectious is the most important factor in determining how many contact tracers need to be deployed. There are potential efficiencies to contact tracing. For example, during the 2014-2016 Ebola outbreak, several states in the U.S. established digital interfaces (web, app) for returning travelers to report their status daily. Where resources allow, public health agencies can call each contact each day; where and when resources are limited, an online system might capture the status of the vast majority of people in quarantine, leaving the public health system to reach out to those who have not reported their status and those who report symptoms or a need for assistance.
The ability to locate contacts and their willingness to be interviewed, quarantined, and to report their status daily is another key factor; the more time this takes, the more contact tracers will be needed. Because people may find the contact tracing process to be inconvenient, it is essential to make easy for people to participate and ensure privacy and confidentiality. Excellent training, strong people skills, and supportive and expert supervision of contract tracers is essential for success. Public education campaigns will be important to inform people about what the process entails, what it means if someone is identified as a contact, and the importance of participation to controlling the pandemic and keeping society open.
Although we have some information about infectivity and are learning more daily, we need to know more about how often casual contact spreads infection. For example, if a brief interaction with a store clerk is unlikely to transmit infection, less time is needed to assess incidental contacts and more time on the close contacts. If asymptomatic people infected with the virus commonly spread it, contact tracing becomes much more challenging.
Emerging evidence suggests that most people with SARS-CoV-2 infection do not spread it to anyone else, but that in some instances it spreads widely (e.g., during choir practice where singing can spread infection, or, potentially, from contaminated surfaces). Investigating these occurrences, which may include “superspreading” events, requires highly specialized skills, and may be assisted by newer technologies. If most contact tracing will require an army of contact tracers, investigating and stopping spread during these large-scale events requires the elite troops of contact tracing – experienced disease detectives from the Centers for Disease Control and Prevention and state and local health departments. This is a separate workforce which should advise on more routine contact tracing but be available to deploy immediately any time there is a potential superspreading event.
The number of contact tracers needed has been the subject of considerable discussion. In Wuhan, China, there were 9,000 contact tracers for a population of 11 million, or roughly one per 1,000. In Singapore, with a case rate more than 50 times lower than the rate in Wuhan, there have been approximately 1,000 contact tracers for a population of 5.6 million, or 1 per 5,600 population. Above a certain case rate, contact tracing becomes both overwhelming and inefficient, since there are so many potential sources and exposures.
For a hypothetical population of 1 million with 40 new cases per day, 8 contacts per case, and moderately strong efficiency gains and good participation by cases and contacts, the number of tracers needed might be on the order of 300. Nationally at this case rate, this would translate into approximately 100,000 contact tracers and their supervisors. Singapore is identifying 30-40 contacts per case, a rate that, with this incidence, would require at least 300,000 contact tracers. This estimate does not include additional staff and organizations needed to provide for the housing, support, and services for cases being isolated and contacts being quarantined, nor the staff for more intensive investigations as described above. This is a theoretical number which should be adjusted based on actual experience. If contact tracing and other measures are successful in controlling the pandemic, then new cases could decline over time; however, it is critically important to maintain capacity for these activities in the event of rebound outbreaks and increases in new cases.
Annex III
Notes
- Ma, J. (2020, March 13). Coronavirus: China’s first confirmed Covid-19 case traced back to November 17. South China Morning Post, Retrieved from https://bit.ly/2XEHeUh
- Pleasance, C. (2020, March 25). The world shuts down: Map shows how a third of the global population – 3BILLION people – are now under coronavirus lockdown. The Daily Mail, Retrieved from http://dailym.ai/2VBRhab
- Connor P. (2020, April 1). More than nine-in-ten people worldwide live in countries with travel restrictions amid COVID-19. Pew Research Center, Retrieved from https://pewrsr.ch/2VzTeUl
- Gottlieb, S, Rivers, C, McClellan, M, Silvis, L, and Watson, C. (2020, March 29). National coronavirus response: A road map to reopening. American Enterprise Institute, Retrieved from https://bit.ly/2XF1t4g
- Emanuel, Z, Tanden, N, Spiro, T, Conner, A, DeGood, K, Simpson, E, Rapfogel, N, and Calsyn, M. (2020, April 3). A National and State Plan To End the Coronavirus Crisis. Center for American Progress, Retrieved from https://ampr.gs/2XFdJlp
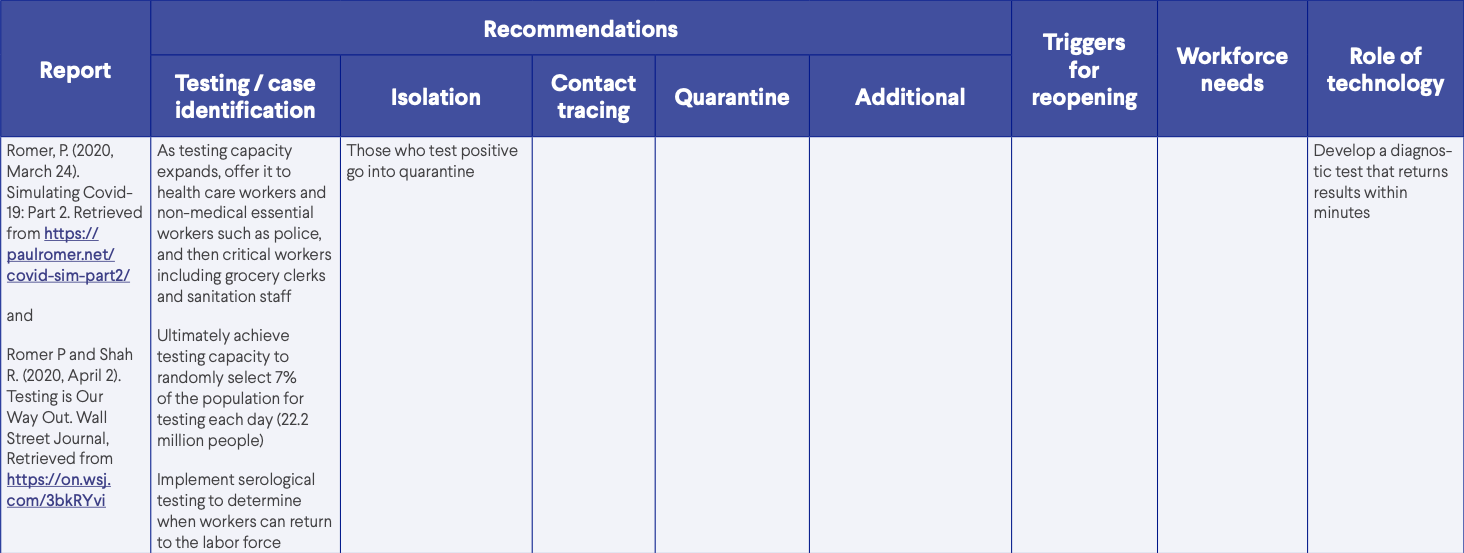
- Romer, P. (2020, March 24). Simulating Covid-19: Part 2. Retrieved from https://paulromer.net/covid-sim-part2/
- Matone, M and Marshall, D. (2020, April). Policy Review: Literature to Inform COVID-19 Mitigation Following Community Reopening. Children’s Hospital of Philadelphia, Retrieved from https://bit.ly/2RF7ASb
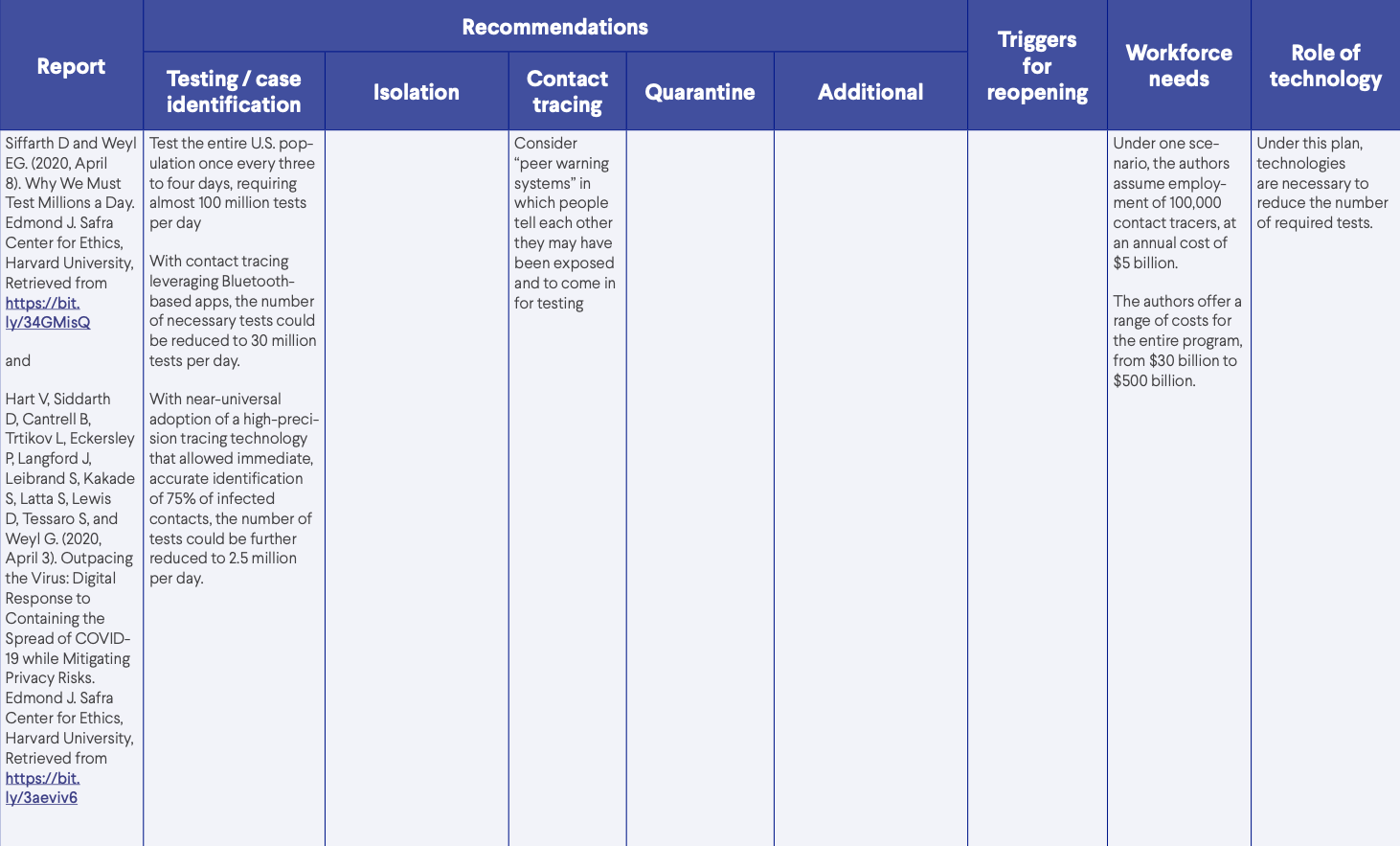
- Edmond J. Safra Center for Ethics, Harvard University. (2020). COVID-19 Response White Papers. Retrieved from https://bit.ly/2KcuY5r
- U.S. Centers for Disease Control and Prevention. (2020). Nursing Home Care. Retrieved from https://bit.ly/2KfSxKB
- Resolve to Save Lives. (2020, April). When and How to Reopen After COVID-19. Retrieved from https://bit.ly/2VdFmjN
- Resolve to Save Lives. (2020, April). When and How to Close due to COVID-19 Spread. Retrieved from https://bit.ly/3airs41
- https://www.youtube.com/watch?v=qal6C9oTbsQ
- Alltucker, K. (2020, April 2). Labs are testing 100,000 people each day for the coronavirus. That’s still not enough. USA Today, Retrieved from https://bit.ly/2KctrfY
- Bennhold, K. (2020, April 6). A German Exception? Why the Country’s Coronavirus Death Rate Is Low. New York Times, Retrieved from https://nyti.ms/3bg9fWa
- Liu J, Liao X, Qian S, Yuan J, Wang F, Liu Y, et al. (2020, June). Community transmission of severe acute respiratory syndrome coronavirus 2, Shenzhen, China, 2020. Emerg Infect Dis. Retrieved from https://doi.org/10.3201/eid2606.200239
- U.S. Centers for Disease Control and Prevention. (2020, April 14). Characteristics of Health Care Personnel with COVID-19 — United States, February 12–April 9, 2020. MMWR Morb Mortal Wkly Rep. Retrieved from: http://dx.doi.org/10.15585/mmwr.mm6915e6
- U.S. Centers for Disease Control and Prevention. (2020). Nursing Home Care. Retrieved from https://bit.ly/2KfSxKB
- Ivory, D, Bogel-Burroughs, N, and Smith, M. (2020, April 14). Coronavirus Outbreak at Virginia Nursing Home Spirals Out of Control as 45 Die. New York Times, Retrieved from https://nyti.ms/2XFJxqk
- Dinki, T. (2020, April 14). Nursing home residents account for almost half of Western New York’s COVID-19 deaths. WBFO, Retrieved from https://bit.ly/2z6zHn8
- Corley, C. (2020, April 13). The COVID-19 Struggle In Chicago’s Cook County Jail. NPR, Retrieved from https://n.pr/2XFJKtC
- Cohn, D’Vera and Passel, J. (2018, April 5). A record 64 million Americans live in multigenerational household. Pew Research Center, Retrieved from https://pewrsr.ch/2ykahlD
- U.S. Centers for Disease Control and Prevention. (2020). Healthcare Facility Guidance, Retrieved from https://bit.ly/3cg11xw
- McMichael TM, Clark S, Pogosjans S, et al. (2020, March 27). COVID-19 in a Long-Term Care Facility — King County, Washington, February 27–March 9, 2020. MMWR Morb Mortal Wkly Rep 2020;69:339-342. Retrieved from http://dx.doi.org/10.15585/mmwr.mm6912e1
- McMichael TM, Currie DW, Clark S, Pogosjans S, Kay M, Schwartz NG, Lewis J, Baer A, Kawakami V, D.V.M, Lukoff MD, Ferro J, Brostrom-Smith C, M.S.N. et al. (2020, March 27). Epidemiology of Covid-19 in a Long-Term Care Facility in King County, Washington. New England Journal of Medicine, Retrieved from https://bit.ly/2VCOzRT
- Frieden, T. (2020, March 8). Former CDC director: It’s time to restrict visits to nursing homes. CNN, Retrieved from https://cnn.it/2XHZcoP
- Hoe GAN, W., Wah LIM, J., & KOH, D. (2020). Preventing intra-hospital infection and transmission of COVID-19 in healthcare workers. Safety and Health at Work, Advance online publication. https://doi.org/10.1016/j.shaw.2020.03.001
- Xinghui K. (2020, March 28). Why are there so few coronavirus infections in Singapore’s health workers? South China Morning Post, Retrieved from https://bit.ly/2VeDIyA
- Ng, K., Poon, B. H., Kiat Puar, T. H., Shan Quah, J. L., Loh, W. J., Wong, Y. J., Tan, T. Y., & Raghuram, J. (2020). COVID-19 and the Risk to Health Care Workers: A Case Report. Annals of internal medicine, L20-0175. Advance online publication. https://doi.org/10.7326/L20-0175
- Fox, M. (2020, April 13). ‘We need an army’: Hiring of coronavirus trackers seen as key to curbing disease spread. STAT, Retrieved from https://bit.ly/34MXDrl
- Newton, C. (2020, April 10). Why Bluetooth apps are bad at discovering new cases of COVID-19. The Verge, Retrieved from https://bit.ly/3beaEwF
- World Health Organization. National Health Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19). Retrieved from https://bit.ly/3euMno7
- Reuters. (2020, April 1). China reports fewer coronavirus infections, tallies asymptomatic cases. Retrieved from https://reut.rs/2VuVw7m
- Chang R, Che C, Bloomberg. (2020, March 19). China’s coronavirus epicenter reaches milestone of zero new cases. Fortune, Retrieved from https://bit.ly/3ahHtXY
- Buchwald E. (2020, April 6). What we can learn from South Korea and Singapore’s efforts to stop coronavirus (besides wearing face masks). MarketWatch, Retrieved from https://on.mktw.net/2Khp4Qt
- U.S. Centers for Disease Control and Prevention. (2020, April 3). Interim Clinical Guidance for Management of Patients with Confirmed Coronavirus Disease (COVID-19), Retrieved from https://bit.ly/2yji7fa
- He, X., Lau, E.H.Y., Wu, P. et al. (2020, April 15). Temporal dynamics in viral shedding and transmissibility of COVID-19. Nat Med Retrieved from: https://doi.org/10.1038/s41591-020-0869-5
- McCall MC, Nunan D, Heneghan C. (2020, April 6). Is a 14-day quarantine effective against the spread of COVID-19? University of Oxford, Centre for Evidence-Based Medicine, Retrieved from https://bit.ly/2VB4PTd
- Webster RK, Brooks SK, Smith LE, Woodland L, Wessely S, Rubin GJ. How to improve adherence with quarantine: Rapid review of the evidence. Retrieved from https://bit.ly/3epAWhv
- Long A. (2020, March 31). What the U.S. Can Learn from Asia’s Coronavirus Response. Wilson Center, Retrieved from https://bit.ly/3bhYenj
- Republic of Korea, Ministry of Health and Welfare. About COVID 19: Patient Treatment & Management. Retrieved from https://bit.ly/34Km5tf
- Centers for Medicare and Medicaid Services. National Health Expenditure Data, Highlights. Retrieved from https://go.cms.gov/3abiZQd
- Prevent Epidemics. Readyscore Map. Retrieved from https://preventepidemics.org/map/
Suggested citation: Frieden T, Shahpar C, McClelland A, and Karpati A. (2020, April). Box It In: Rapid Public Health Action Can Box In Covid-19 and Reopen Society. Resolve to Save Lives, Retrieved from https://preventepidemics.org/coronavirus/resource/box-it-in/©2020 by Vital Strategies, Inc. through its Resolve To Save Lives initiative. All materials that are publicly posted are available for use as long as they are attributed to Resolve to Save Lives, an initiative of Vital Strategies, and not used for profit-seeking purposes. Vital Strategies is a nonpartisan, nonprofit, 501(c)(3) charitable, educational, and scientific organization.
Download Resources:
-
Box It In: Rapid Public Health Action Can Box in COVID-19 and Reopen Society
(493.79 KB)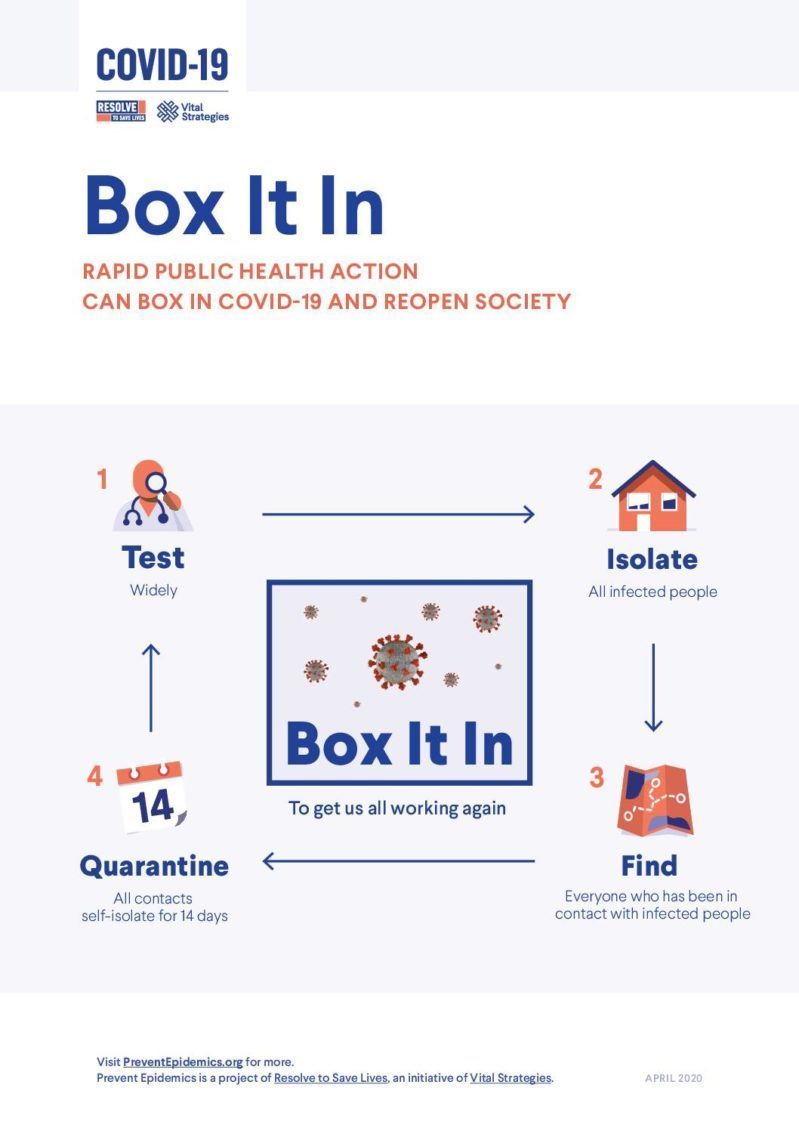
-
Press Release: Former CDC Director and Resolve to Save Lives President and CEO, Dr. Tom Frieden, Releases Detailed Action Plan to Contain the COVID-19 Pandemic and Gradually Reopen Society
-
Briefing Video: Virtual Media Availability with Dr. Tom Frieden April 17, 2020
-
Encerclons la COVID-19
French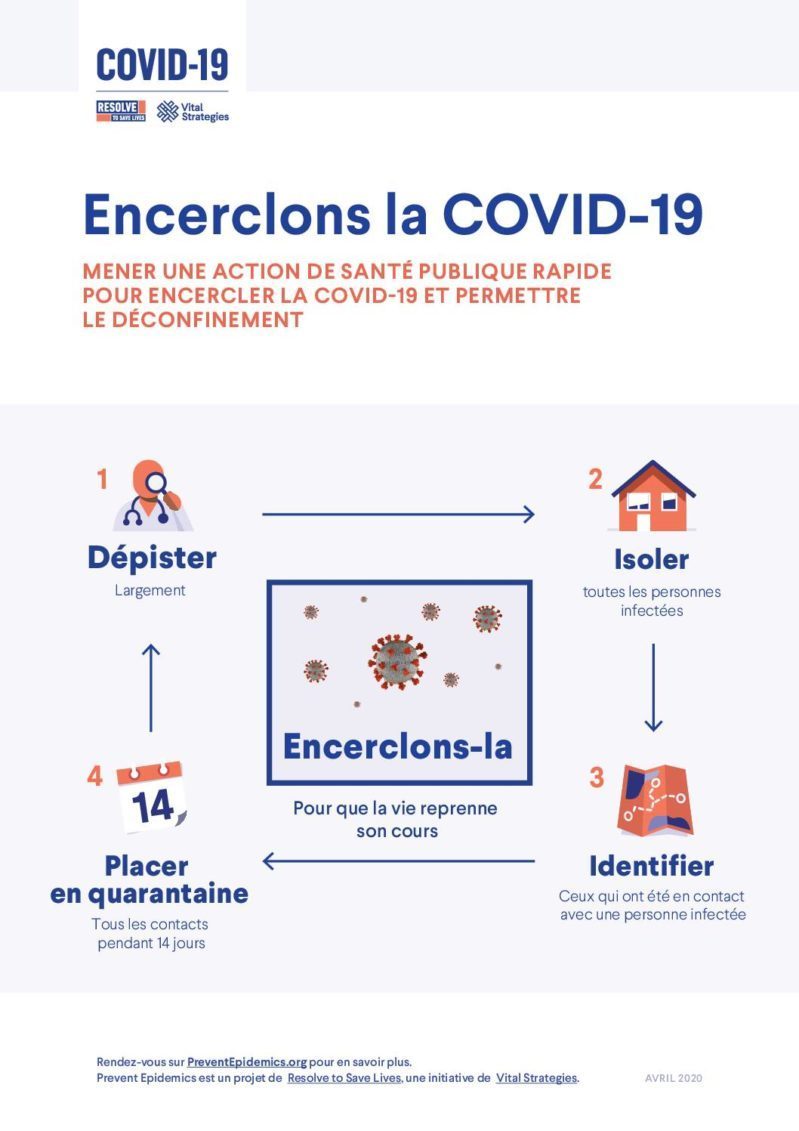
-
Contención del virus
Spanish