Data insight:
Nowcasting in the context of COVID-19
Nowcasting is a combination of “now” and “forecasting” and is traditionally associated with the fields of meteorology and economics. It involves the use of data to understand the current situation and forecast the immediate future. This approach has been applied to a variety of information analyses including weather reports and Gross Domestic Product projections to provide timely information than can be used to inform action.
In the COVID-19 pandemic, one application of nowcasting is the estimation of the basic reproduction number (Ro) also known as the basic reproductive ratio. This is defined as the expected number of secondary infections arising from a single individual during his or her entire infectious period in a population of susceptible people. The reproductive number is one way to estimate the transmissibility of a specific pathogen such as SARS-CoV-2, and has important implications for disease control. When Ro is greater than 1, a disease continues to spread since each infected person will spread it to more than one person, on average. When Ro equals 1, then each existing infection would on average cause one new infection. When Ro is less than 1, fewer and fewer people will be infected over time and the disease can be controlled.
Ro is driven by three main parameters including the duration of contagiousness, the rate of contact between infected and susceptible persons (contact rate), and the likelihood of infection when contact is made. One important limitation to the concept of Ro is that it does not capture the heterogeneity of transmission among infected people, and two pathogens with identical Ro estimates may have markedly different patterns of transmission. A main objective of disease control measures is to drive down Ro to a value below 1 by implementing interventions that affect the three parameters above. For example, isolation, quarantine and physical distancing measures reduce the contact rate between the infected and susceptible. This real-life observed reproductive number is called the effective reproductive number (R or Rt for a given time period) which can change and be monitored as the number of susceptible members of a population changes due to changing behaviors (e.g. physical distancing), treatment and vaccination. Logically, if near real-time estimates of Ro could be produced, then one could see the impact of public health interventions on the spread of COVID-19 and better understand the current status of disease transmission.
In the ongoing pandemic, several groups have recently released frequently updated Ro or Rt estimates. The Centre for the Mathematical Modelling of Infectious Diseases at the London School of Hygiene & Tropical Medicine provides current estimates of the effective reproductive number and doubling time (most recent time it has taken for case counts to double) estimates by country. In the figure below, the current Ro in most countries in the world is above 1, indicating that the disease will continue to spread.
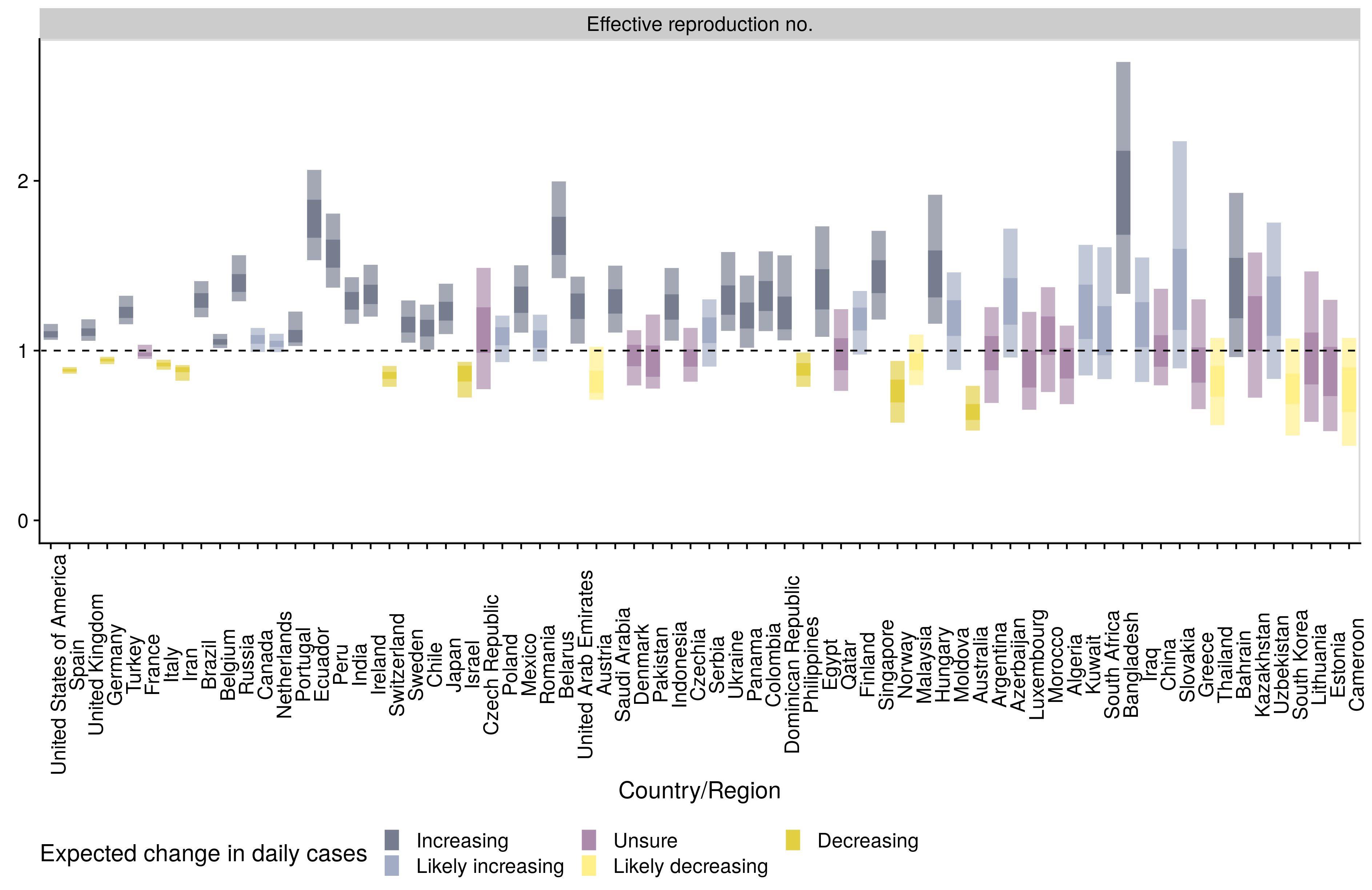
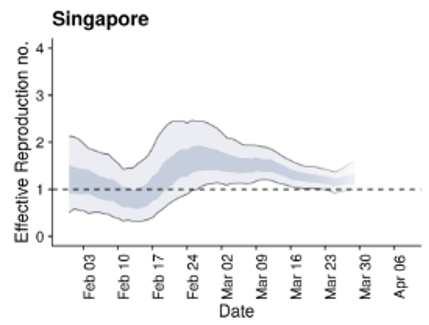
Singapore and South Korea were able to implement measures to drive down their Ro below the threshold value of 1, allowing them to control disease spread. In both areas there has been a rebound of Ro above 1, largely due to residents who are infected returning to their home country leading to new chains of disease transmission.
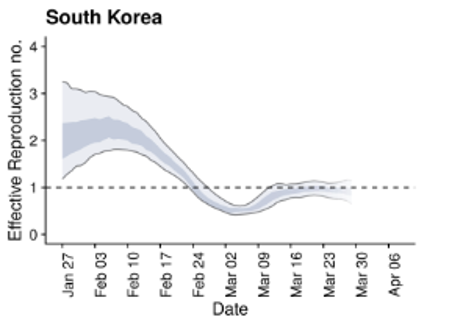
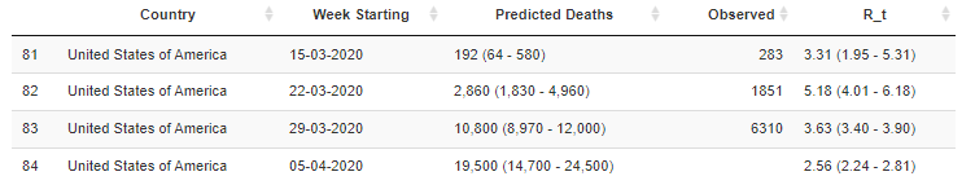
Similarly the MRC Center for Global Infectious Disease Analysis at the Imperial College of London has started releasing COVID-19 weekly forecasts. In these forecasts, they classify the COVID-19 situation in countries as stabilizing, growing slowly or growing rapidly, using estimates of the reproduction number. They also provide estimates of the current effective reproduction number for countries around the world (figure below).
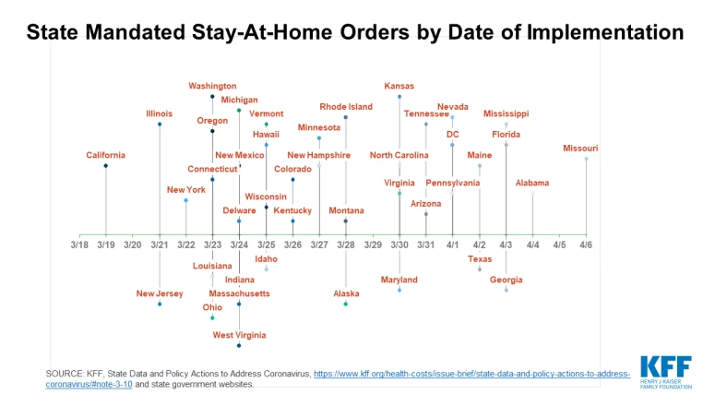
In their estimates of the reproduction number in the United States by week, the number declined from 5.2 the week of March 22 to 2.6 the week of April 5. This corresponds to the time period that most states implemented shelter-in-place orders (see Figures below), but, importantly, remains far above 1.
One group examined the instantaneous reproduction number (Rt) of COVID-19 in Beijing, Shanghai, Shenzhen, Wenzhou, and the ten Chinese provinces that had the largest number of confirmed COVID-19 cases.
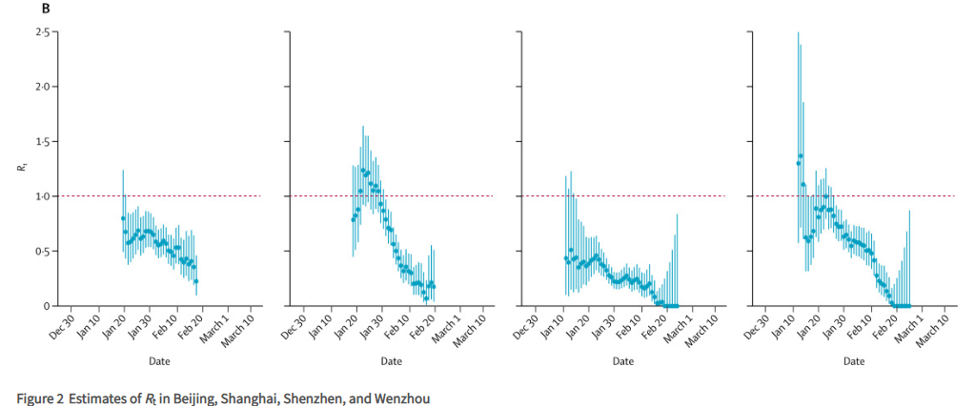
The authors analyzed Rt and implementation of containment measures and mobility data and found that the first wave of COVID-19 outside of Hubei abated because of aggressive non-pharmaceutical interventions. The decline in the reproduction number in the four selected cities correlated with the decrease in intracity traffic volumes recorded by Baidu.
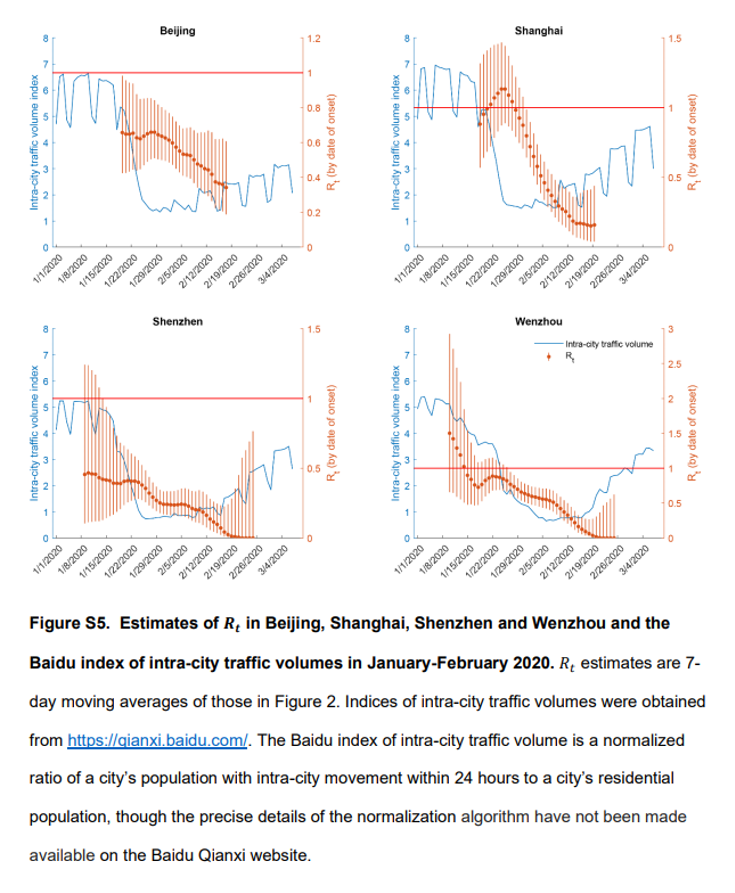
Overall, the authors concluded that the comprehensive package of non-pharmaceutical interventions substantially reduced transmissibility of COVID-19 across China. The daily number of local COVID-19 cases has dropped substantially, to nearly zero in areas outside Hubei since late February; however, a second wave of COVID-19 transmission is possible because of viral reintroduction that has been increasing since March 2020, as well as viral transmissibility that might rebound with the gradual resumption of economic activities and thus normal levels of social mixing. The authors recommend close monitoring of the instantaneous effective reproduction number and real-time tuning of policy interventions to ensure manageable additional waves.
Similarly, the Institute for Disease Modeling in Washington State, USA used estimates of the effective reproduction number to assess whether physical distancing measures and subsequent changes in population mobility are related to reductions in COVID-19 transmission. They report that before behavior change on March 1, 2020 the effective reproduction number was 2.7 (+ 0.9). In mid-March, Washington State instituted increasing levels of separation policies, including closing schools and canceling mass gatherings. By March 18, after these measures were in place, the effective reproduction number had fallen to 1.4 (+ 0.2) based on epidemiological data alone.After adding in additional mobility data, they report that the nowcast of the effective reproduction number became more precise at 1.3 (+ 0.07).
Monitoring the reproduction number over time has promise as a tool to assess the impact of interventions and trigger actions to implement or relax physical distancing measures. However, the estimates of reproduction number for a specific location and time period are not consistent across models and although Ro is easy to understand it is difficult to quantify. One recent article on the complexity of the reproductive ratio concluded that it “must be estimated, reported, and applied with great caution because this basic metric is far from simple”. For example, for the week of March 29, 2020, the LSHTM model estimated the effective reproduction number in the United States to be 1.2
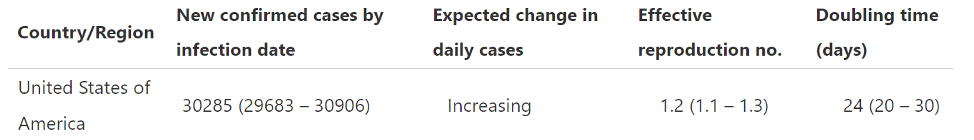
During the same period, the Imperial College models (they use 3 and summarize) estimated the reproduction number to be 3.63. These point estimates are very different, and it is probably more useful to look at the trends within each model than to compare reproduction numbers across models. Moving forward, these models will continue to be refined and augmented with additional types of information to inform our response to COVID-19.
Topics in depth
BCG and COVID-19
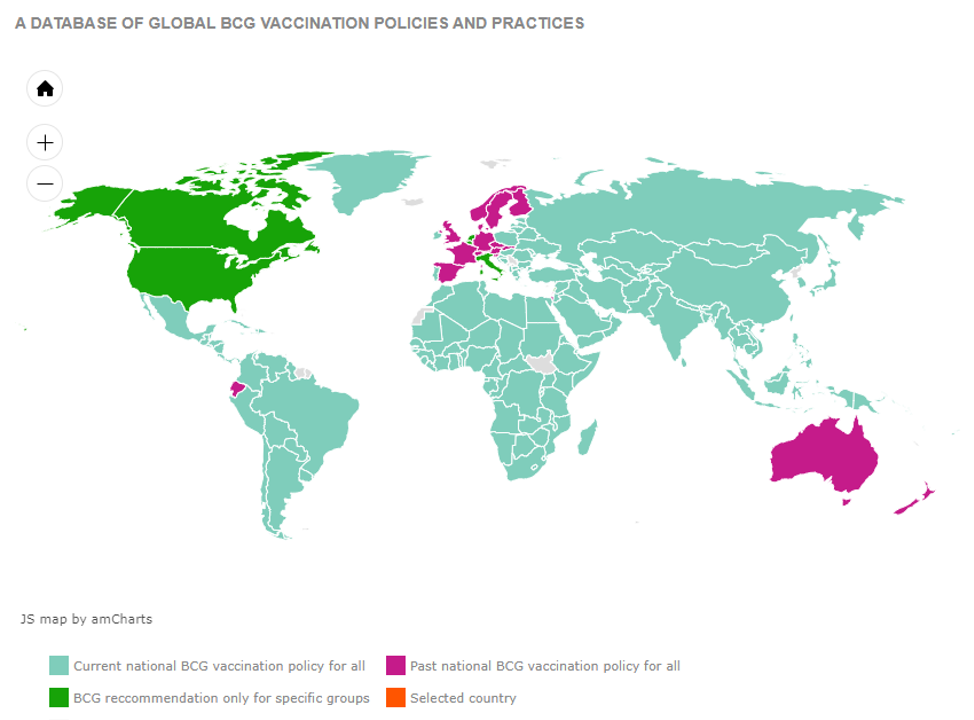
Myriad factors may contribute to vast observed differences in the burden of COVID-19 between countries. It has been noted that COVID-19 morbidity and mortality appear to be higher in countries in which universal vaccination against tuberculosis at birth with Bacillus Calmette-Guérin (BCG) vaccine is not recommended (for example Italy, Spain, France, and the UK) than in those in which it is (for example Japan and South Korea). The rationale behind examining this relationship and conducting clinical trials to evaluate the impacts of BCG vaccination on the burden of COVID-19 merits discussion.
BCG vaccination is used to prevent TB severe forms of the disease in children, such as tuberculosis meningitis. Since its introduction 100 years ago, more than 3 billion people have received BCG vaccination, making it the most-used vaccine in history. Universal childhood BCG vaccination continues to be recommended in most countries; other countries where the incidence of TB has fallen no longer recommend universal BCG vaccination, and some countries have never had a universal BCG vaccine policy.
In recent decades, there have been hypotheses that BCG vaccination may be associated with greater reductions in morbidity and mortality than would be expected from its effects on TB alone. BCG vaccination has been associated with reductions in child morbidity and mortality, possibly through reduction of the incidence of severe non-tuberculosis respiratory infections. The incidence of respiratory infections in the elderly was reported to have been reduced by repeated BCG vaccination in one study. Data from human, animal, and in vitro studies indicate that these effects may be due to non-specific boosting of immunologic function. However, other studies have failed to demonstrate an effect of BCG vaccination on various outcome measures. A range of variables, including country of birth, age of vaccination, type of BCG vaccine, and nature of subsequent immunologic challenge may modify any protective effects. Our understanding of the impact of BCG vaccination on immunologic function and population health continues to be refined.
Three observational studies have found correlations between universal BCG vaccination and the burden of COVID-19. One study found lower COVID-19 mortality in countries with universal BCG vaccination after excluding low-income countries given concern for case and death ascertainment biases. A second study with similar findings adjusted for each country’s relative position on the epidemic curve, and a third study showed flatter incidence and fatality growth curves in countries with universal BCG vaccination during the initial period of the pandemic, before the introduction of divergent control measures. These studies also attempted to control for other potential confounders of observed associations between BCG vaccination and COVID-19, but factors such as comorbidities, co-infections, and differential uptake of non-pharmaceutical interventions are difficult to address. The strength of evidence from these, as from any, ecological studies, is limited. Nonetheless, these findings, together with existing data on the protective effects of BCG vaccination, have spurred the launch of clinical trials to investigate whether BCG vaccination may decrease COVID-19 incidence and fatality rates. A randomized control trial of the impacts of BCG vaccination on COVID-19 incidence and severity among healthcare workers in Australia is being launched, and a similar study is being planned in Germany.
Impact of dosage (inoculum) on COVID-19 severity
Healthcare workers (HCW) are a significant proportion of confirmed COVID-19 infections. Although frontline HCW are at higher risk of coming into contact with SARS-CoV-2 than those who are able to practice physical distancing, the number of SARS-CoV-2 virions present at exposure (here referred to as the exposure dose and also known as the inoculum) may also influence the risk of infection and disease severity.
The infectious dose, or the median number of infectious organisms needed to establish infection in most individuals, is a concept relevant to the relationship between exposure dose and the likelihood of infection. The infectious dose of SARS-CoV-2 has not yet been established. Challenge studies of both humans and non-human animals have helped define the infectious doses for a wide range of pathogens; for SARS-CoV-2, animal data is not yet available and human infectivity studies would pose insurmountable safety and ethical challenges. However, there are relevant data on related coronaviruses and other respiratory pathogens. A human challenge study on influenza showed that higher viral inoculums more effectively produce infection and clinical influenza symptoms compared than lower inoculums. Mouse models of SARS-CoV (the coronavirus that causes SARS) have shown that replication in the lungs and nasal turbinates correlates with exposure dose. And during the 2002 SARS epidemic, among 79 SARS patients who shared a high-rise residential complex in Hong Kong, infection was more likely and the initial viral load was higher among those who lived close to the index case. Based on these data as well as general principles on the interplay between infectious pathogens and host immune defenses, it is likely that higher SARS-CoV-2 exposure doses are more likely to cause infections than lower exposure doses. This does not, however, prove that exposure dose is associated with illness severity.
Another concept in the relationship between the amount of SARS-CoV-2 and COVID-19 illness severity is that of viral load, or the amount of virus carried by an individual. For both SARS-CoV and MERS-CoV (the viruses that cause SARS and MERS, respectively), high viral loads have been associated with mortality. Data on the relationship between SARS-CoV-2 viral load and COVID-19 severity are emerging: median initial SARS-CoV-2 viral loads from 23 patients in Hong Kong were not significantly different between mild and severe cases. In Italy, viral loads measured at diagnosis were not different between asymptomatic and symptomatic COVID-19 patients. However, initial viral load may not correlate with subsequent viral kinetics and illness severity, especially given the importance of host factors in determining the course of illness. In the aforementioned study of SARS patients in Hong Kong, although the severity of illness upon diagnosis was not correlated with viral load or with living distance from the index case, the death rate was positively correlated with higher subsequent viral loads and was higher among those who lived close to the index case. Among 76 COVID-19 patients in China, those with severe disease tended to have higher viral loads over the course of illness. The first published time-series analysis of SARS-CoV-2 viral kinetics and illness severity from Europe describes three trajectories: a pauci-symptomatic course with high early and later waning viral load; secondary clinical worsening around day 10 despite decreasing viral load; and a consistently high viral load with multi-organ failure.
In summary, it is likely but not proven that SARS-CoV-2 exposure dose influences the likelihood of an exposed person becoming infected, and there is evidence of an association between high viral loads later in the course of illness and COVID-19 severity. The missing and potentially more difficult question to answer is whether there is a relationship between exposure dose and subsequent viral load kinetics and/or illness severity. As a last point, there is evidence of high nasopharyngeal SARS-CoV-2 viral loads in COVID-19 patients. The presence of viral RNA does not necessarily indicate infectivity; these data warrant consideration of the hazard this may pose to HCW and contacts of COVID-19 patients, especially given the possibility – as yet unproven – that a higher exposure dose may increase disease severity.
Article highlights
Epidemiology
Coronavirus Disease 2019 in Children — United States, February 12–April 2, 2020.
(MMWR 6 April 2020)
- As of April 2nd, less than 2% of cases currently being reported in the US are among those under 18 years old, and 32% of these are among children 15 or older.
- A large majority, 91% of children testing positive, had a known family or community contact who had documented COVID-19.
- Fewer children under 18 than adults with COVID-19 report fever, cough, and shortness of breath, however data for symptoms at presentation is incomplete.
Community Transmission of SARS-CoV-2 at Two Family Gatherings — Chicago, Illinois, February-March 2020
(MMWR 8 April 2020)
- Although the index patient, who reported out-of-state travel prior to symptom onset, suffered only mild symptoms and was tested as part of an epidemiologic investigation, there were 3 deaths reported as a result of this transmission chain.
- This type of disease spread supports current widespread state and local guidelines prohibiting private and public gatherings and advising residents to stay at home and shelter in place to limit ongoing transmission.
- The study is limited by lack of genetic epidemiology to confirm relatedness of infections, as some persons reported contact with more than 1 known SARS-CoV-2 case.
- Social distancing will remain a key element in addressing the current pandemic, and additional studies evaluating the specific modes of person-to-person transmission at social gatherings will shed light on how entities/jurisdictions can tighten or loosen restrictions as soon and safely as possible.
Hospitalization Rates and Characteristics of Patients Hospitalized with Laboratory-Confirmed Coronavirus Disease 2019 — COVID-NET, 14 States, March 1–30, 2020
(MMWR 8 April 2020)
- Overall hospitalization rate during March was 4.6/100,000. Hospitalization rate was lowest for pediatric patients and increased with age. Rates per 100,000 persons are as follows: 0-4 yrs: 0.3; 5-17 yrs: 0.1; 18-49 yrs: 2.5; 50-64 yrs: 7.4; ⩾65 yrs: 13.8.
- Of all patients hospitalized with COVID-19, 0.4% were 0-17 yrs old; 24.7% were 18-49 yrs old; 31.1% were 50-64yrs old; and 43.4% were ⩾65 yrs old.
- When compared to seasonal influenza, COVID-19 is resulting in similar hospitalization rates for those under 18 (0.1/100,000 vs 0.1/100,000), but much higher rates in older adults (e.g. for those ⩾85 yrs, 17.2/100,000 vs 2.2-5.4/100,000).
- In 89% of hospitalizations for which data was available (n=178), the patient had at least 1 underlying condition. The most common underlying condition overall was hypertension (49.7%), followed by obesity (48.3%), Metabolic conditions including diabetes mellitus (36.1%) and chronic lung disease (34.6), some of which are associated with severe illness from COVID-19.
Geographic Differences in COVID-19 Cases, Deaths, and Incidence —United States, February 12–April 7, 2020
(MMWR 10 April 2020)
- Across the US, geographic differences exist in the number of cases of COVID-19, number of deaths, cumulative incidence, and changing incidence. Some of this variation can be explained by differences in the timing of introduction of cases and transmission.
- Population density likely has an effect on transmission and cumulative incidence given the primary transmission of SARS-CoV-2 by respiratory droplets. Availability of testing, and exposure of vulnerable populations, characteristics of the context of initial case introduction, are other probable contributors to these findings.
- Continued monitoring of jurisdictional data is necessary to guide local efforts to assess and mitigate risk, and to guide strategic healthcare resource allocation.
Neutralizing antibody responses to SARS-CoV-2 in a COVID-19 recovered patient cohort and their implications
(Preprint-MedRxiv 30 March 2020)
- NAbs obtained from plasma of 5 recovered COVID-19 patients displayed neutralization, or clearing, of SARS-CoV-2 PsV infection of 293T/ACE2 cells, the known target binding site of SARS-CoV-2. (PsV, or pseudovirus, is an adapted virus for lab setting)
- Despite similarities in spike proteins of SARS-CoV and SARS-CoV-2, antigenicity of the viruses is different and specific. Regardless of cross-binding, NAbs from SARS-CoV-2 did not neutralize SARS-CoV.
- For 6 patients, the authors obtained multiple samples from different times during the course of disease. Study of these samples showed that NAb titer levels were low prior to day 10 of disease. The levels rose above “low” at day 10-15, and remained stable at these higher levels thereafter.
- About 30% of patients in the cohort, despite having recovered, had low levels of SARS-CoV-2-specific NAbs. 10 of these, or 5.7% of the cohort, had undetectable levels. Nevertheless, disease duration was similar irrespective of NAb titers. One major limitation is the lack of viral load data to correlate with NAb levels.
- Elderly (60-85 yrs) and middle-aged (40-59 yrs) recovered patients had higher levels of NAb titer than younger patients. This may mean that higher levels of NAbs confer better outcomes for the elderly, however no information is available on the NAb titers of severely ill or deceased elderly/middle aged patients for comparison. This point is not addressed by the article. It may also indicate higher innate immune response leading to more severe disease through cytokine activation and immune pathways (this was shown to be plausible in primate studies of SARS-CoV)
The relationship of COVID-19 severity with cardiovascular disease and its traditional risk factors: A systematic review and meta-analysis
(Preprint-MedRxiv 5 April 2020)
- Eligible studies included a range of study designs, adult patients only, and were published in English. Outcomes of interest included severe COVID-19 (all-cause mortality, ICU admission, ARDS, or the need for mechanical ventilation). Potential risk factors included pre-existing cardiovascular disease (CVD), age, sex, smoking, hypertension, and diabetes.
- 373 potentially eligible studies were identified, 15 were included. Most were from China. A total of 51,845 COVID-19 patients were included; 9,066 had severe disease. Older age was associated with severe COVID-19, with a RR >5 in those 60-65 years of age versus those under 50 years of age.
- In univariate analyses, other factors significantly associated with severe COVID-19 were male sex (14 studies; pooled RR=1.70; 95% CI 1.52-1.89), hypertension (10 studies; 2.74; 2.12-3.54), diabetes (11 studies; 2.81; 2.01-3.93), and CVD (9 studies; 3.58; 2.06-6.21). Smoking was not found to be significantly associated with severe COVID-19 (3 studies; 2.01; 0.83-4.86).
- Meta-regression analysis showed that the elevated risk of severe COVID-19 associated with increased age was made greater if comorbidities were present, but not to the level of statistical significance, suggestive of confounding by age. A similar non-significant effect of male sex on the risk of severe COVID-19 associated with CVD was observed.
- There was inadequate evidence to suggest protective or harmful effects of renin-angiotensin system inhibitors. Only one study reported on their use: 30% of the patients in that study had hypertension, and only 5% of those were prescribed medications in that class.
Predictors of Mortality for Patients with COVID-19 Pneumonia Caused by SARS-CoV-2: A Prospective Cohort Study
(ERJ 1 April 2020)
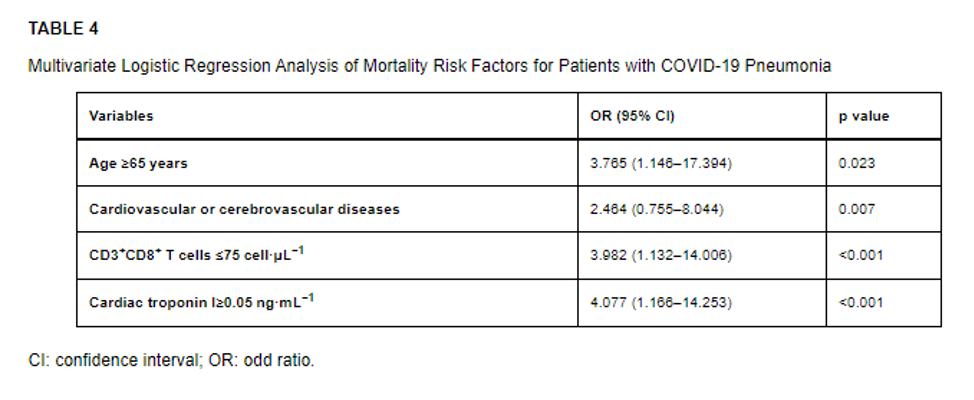
- The authors conducted a prospective cohort study of 179 patients hospitalized with COVID-19 pneumonia at a single site in Wuhan and sought to identify risk factors associated with death.
- Multivariate analysis revealed four risk factors for death as shown in the table below.
Clinical features
Baseline Characteristics and Outcomes of 1591 Patients Infected With SARS-CoV-2 Admitted to ICUs of the Lombardy Region, Italy (JAMA 6 April 2020)
- Among these patients admitted to the ICU for severe COVID-19, ICU mortality was higher in older patients as compared to younger patients (15% for <63 years vs. 36% for >= 63 years). 58% of patients remained in the ICU at the end of the time disposition was examined.
- When looking at PaO2/FiO2 ratio, measure of oxygenation in the blood over oxygen being delivered, which is used to define acute respiratory distress syndrome (ARDS), all of the mechanically ventilated patients had mild to moderate ARDS with the Pa02/Fi02 ratio range from 114 – 220 (mean 160). 1% of patients were treated with ECMO.
- At least one underlying comorbidity was present in 68% of ICU admissions, with hypertension being the most common. Patients with hypertension in this group were older and required higher levels of PEEP, however they had similar FiO2 requirements. The second most common comorbidity was cardiovascular disease.
Management
Compassionate Use of Remdesivir for Patients with Severe Covid-19
(NEJM 10 April 2020)
- Industry-sponsored study of the compassionate use of a 10-day course of remdesivir in a cohort of 61 hospitalized COVID-19 patients around the world
- In 53 patients with sufficient data, 68% had improvement in the level of oxygen support required. Overall, 25 patients (47%) were discharged and 7 (13%) died.
- Several ongoing randomized, controlled trials will soon provide more informative evidence regarding the safety and efficacy of remdesivir for Covid-19.
Effectiveness of convalescent plasma is severe COVID-19 patients
(PNAS 6 April 2020)
- The 10 patients included 6 males and 4 females, with a median age of 52.5 yrs (IQR 45-59.5 yrs). Median time to hospital admission was 6 days from disease onset, and median time to CP transfusion from disease onset was 16.5 days (range 10-20).
- All of the study patients were receiving antiviral medications prior to CP transfusion, and 8/10 had received other antimicrobials such as IV antibiotics, IV antifungals, or a combination. 6/10 patients had received systemic corticosteroids. The role of these additional interventions is not clear in patient outcome, and needs to be taken into consideration.
- Presenting symptoms including fever, cough and shortness of breath resolved or improved in the study patients 1-3 days after CP transfusion, and most patients were able to wean their oxygenation requirements. Patients who received CP transfusion 14 days or less after disease onset improved significantly more than those who received the transfusion later. The appropriate timing of CP transfusion requires further study.
- A historical control group established for the purpose of the study among severely ill patients not differing statistically in parameters of interest had overall worse outcomes including 3 deaths (as compared to 3 discharges in the study group); but the authors acknowledge the need for additional evidence from randomized controlled trials.
Fangcang shelter hospitals: a novel concept for responding to public health emergencies. Chen et al, The Lancet. April 2, 2020
(Lancet 2 April 2020)
- These large-scale temporary hospitals transformed existing public venues such as sporting arenas and convention centers into health care facilities triaging, isolating, and caring for mild to moderate severity COVID-19 patients.
- Three key characteristics (rapid construction, massive scale, and low cost) and five core functions (isolation, triage, basic medical care, frequent monitoring with rapid referral, essential living and social engagement).
- They differ from emergency field hospitals in that they isolate patients highly likely to transmit disease – symptomatic but mobile/active, they triage by severity of disease allowing for cohorting and provision of appropriate care, and were considered national standard of care for isolation of mild to moderate COVID cases rather than surge facilities that would later be incorporated into existing healthcare infrastructure.
- To implement, they require large facilities capable of housing and meeting the feeding, sanitation, isolation, and socialization needs of thousands of people. In addition, they require cultural acceptability of shelter isolation and quarantine for individuals likely well enough to be at home.
FAQs
How much do we touch our faces and what does that mean for COVID-19?
Typically, we touch our faces more than we might think. In one small study looking at this behavior, 26 medical students were videotaped over the course of four hours to see how they touched their faces. Students touched their faces an average of 23 times per hour. Nearly half the time (44%) this involved touching mucous membranes (mouth, nose, eyes). Another study examined hand contamination with influenza. This study found that influenza A viruses have the potential to easily survive on the skin surface of hands immediately after contamination but fall substantially after just 30 minutes. Given our high frequency of mouth and nose touching, and viability of virus on hands and fingers, performing hand hygiene is an essential and inexpensive preventive method for breaking the colonization and transmission cycle of infectious diseases such as COVID-19.
Sanitary recommendations for bringing packages into the home
Are there recommendations about sanitary protocols for bringing packages, groceries, and mail into our home? Is there a different protocol for different items?
Although bringing packages, groceries, and mail into your home is not zero-risk, the risk of infection is very low. You should wash your hands after bringing any of these items into the house. Packages have not been touched by warehouse employees for at least 24 hours by the time they reach your home, which greatly lowers the likelihood of infectious virus on the package. The likelihood that the person delivering your package contaminated it is also very low. If you are concerned and want to be extra careful about packages or mail, you can leave them untouched for three days before opening. For groceries, the most important thing is how you do your grocery shopping. Before you take a cart or basket, you should sanitize the handles. Try to touch as few things as possible while in the store. When you get home, wash your hands with soap and water. The reality is that most people who get infected will not get infected by handling their mail or groceries. Most infections will happen when people get too close to others who may be infected. See this article for some practical tips on handling packages, mail and groceries.
Suggested citation: Cash-Goldwasser S, Kardooni S, Cobb L, Bochner A, Bradford E and Shahpar C. In-Depth COVID-19 Science Review April 4 – 10, 2020. Resolve to Save Lives. 2020 April 13. Available from https://preventepidemics.org/covid19/science/review/