Download All Country Data


PMEP equips health security experts with practical, technical and leadership skills
February 29, 2024
Read story
December 18, 2023
Design sprints from the tech world are changing the game in public health

December 20, 2022
A single guide can support all 36 states in contributing to national health security

December 7, 2022
Dedicated preparedness team uses regular communication to support multi-sectoral collaboration
November 16, 2022
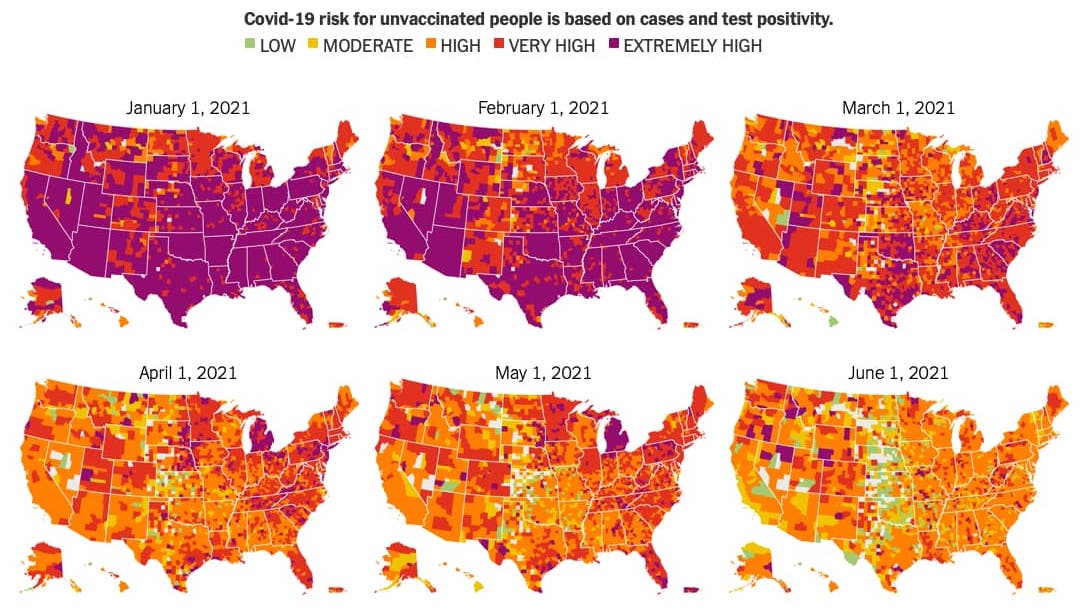
“One stop shop” pairs consistent, data-driven interpretations of risk with recommended precautions

August 19, 2022
Campaigns demonstrate power of transparent communication and trust in public health messaging
July 14, 2022
Mobile-optimized, case-based online courses keep health care workers up to date more effectively.

June 15, 2022
Awareness campaign spotlights COVID long-haulers to increase vaccine uptake

April 13, 2022
A community-focused approach to vaccination in underserved census tracts

March 16, 2022
Time to respond to outbreaks following detection fell from six days to two